“Background: Cannabinoids have attracted significant attention for their potential therapeutic application in cancer research. However, recent studies have reported antitumor activity of cannabidiolic acid (CBDA)-the acidic precursor of CBD-in breast cancer cells, involving modulation of cyclooxygenase signaling. To our knowledge, no investigations have examined the effects of CBDA on RNA expression and signaling pathways in colorectal cancer (CRC) cells. Therefore, we aimed to investigate the effects of CBD, CBDA, and a CBDA-rich Cannabis sativa (C.s). extract on the growth and gene expression in CRC cell lines.
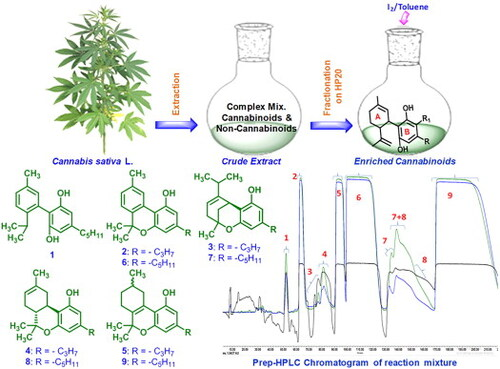
Methods: We assessed cell viability and clonogenic growth of the CRC cell lines HCT116 and DLD1 following treatment with pure CBD, pure CBDA, a CBDA-rich C.s. extract (CBDA/CBD ratio 20:1), and a corresponding mixture of pure CBDA/CBD. RNA sequencing was performed to analyze differentially expressed genes (DEGs) and the cell signaling pathways affected by these treatments.
Results: Of all tested compounds, CBD exhibited the strongest cytotoxic effect in both cell lines, whereas CBDA demonstrated minimal toxicity, particularly in HCT116 cells. Furthermore, we observed a greater inhibitory effect of the CBDA-rich C.s. extract on HCT116 cell growth compared to the CBDA/CBD mixture. RNA sequencing analysis revealed that CBD had the most pronounced impact on gene expression, while CBDA had the least. Notably, treatment with the C.s. extract resulted in a higher number of DEGs than the CBDA/CBD mixture in HCT116. Gene expression analysis indicated an upregulation of the Wnt and Hippo signaling pathways following CBD treatment. Additionally, CBDA, CBD/CBDA (1:20), and the C.s. extract primarily induced metabolic processes in DLD1 cells, suggesting a distinct metabolic response.
Conclusion: Our findings showed that CBD exerts stronger effects on cell survival and gene expression in CRC cells than CBDA, which showed only limited activity. Moreover, the CBDA-rich C.s. extract exhibited greater efficacy than the CBDA/CBD mixture. More research is needed to further elucidate the impact of cannabinoids on CRC cell biology and signaling pathways.”
https://pubmed.ncbi.nlm.nih.gov/41546069
https://link.springer.com/article/10.1186/s42238-026-00391-2