“Breast cancer remains a leading cause of cancer-related morbidity and mortality globally, highlighting the urgent need for novel therapeutic strategies.
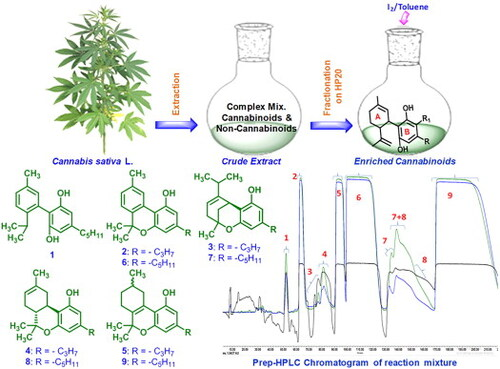
This study investigates the molecular mechanisms underlying the anti-proliferative potential of Cannabis sativa dichloromethane extract (C. sativa DCM) on oxidative stress, apoptosis, and invasion in human breast cancer cells.
Key biomarkers, such as antioxidant enzymes (Superoxide Dismutase (SOD) and Glutathione (GSH)), the transcription factor Nrf2, apoptotic proteins (p53, caspase-8 and 9), metalloproteinase (MMP-1 and MMP-9), and Transforming Growth Factor Beta (TGF-β) were examined. Cytotoxicity was assessed using an MTT assay in the MDA-MB-231 and MCF-7 breast cancer cell lines, with comparisons to normal skin fibroblasts (HS27). Oxidative stress biomarkers were quantified using enzymatic assays and ELISA kits, while apoptotic and anti-metastatic factors were determined by Western blotting.
Results demonstrated that C. sativa DCM extract induced significant cell death in a concentration-dependent manner, with IC50 values of 75.46 ± 0.132 μg/mL for MDA-MB-231 and 78.68 ± 0.50 μg/mL for MCF-7 cells. The extract decreased SOD and GSH levels while increasing p53 and caspase activity, confirming apoptosis activation. Additionally, C. sativa DCM inhibited migration and invasion by downregulating MMP-1, MMP-9, and TGF-β. The anti-proliferative potential of C. sativa DCM in breast cancer cells is mediated through a continuous biological pathway involving oxidative stress modulation, apoptotic signaling, and anti-invasive effects. Phytochemical analysis revealed terpenoids and steroids, including compounds like cannabidiol and tetrahydrocannabinol acid.
These findings suggest that C. sativa DCM extract holds potential as an anti-breast cancer therapeutic and warrants further preclinical and clinical investigations.”
https://pubmed.ncbi.nlm.nih.gov/41516029
“Cannabis sativa L., known in many slang languages as marijuana, bhang, ganja, for instance, is an herbaceous species originating from Central Asia and widely distributed around the world. It has been used as a source of fiber, food, oil, and for its multiple curative properties, including anti-parasitic, antipyretic, antibacterial, antitumor, vermifuge, dermatic, and pain-killing properties for centuries. Phytocannabinoids, derived from cannabis, have shown anti-cancer activity in cell lines”
“Based on these research findings, we concluded that C. sativa DCM extract possesses the potential to inhibit the proliferation of breast cancer cells (MCF-7 and MDA-MB-231), while exhibiting minimal cytotoxic effect on normal skin cells Hs27.”
“Given these conclusive findings, the presence of bioactive phytochemicals in C. sativa DCM can be considered as a potential source of anti-cancer agents.”
https://www.mdpi.com/1422-0067/27/1/152