 “Critically ill patients with sepsis require a multidisciplinary approach, as this situation implies multiorgan distress, with most of the bodily biochemical and cellular systems being affected by the condition. Moreover, sepsis is characterized by a multitude of biochemical interactions and by dynamic changes of the immune system. At the moment, there is a gap in our understanding of the cellular, genetic, and molecular mechanisms involved in sepsis.
“Critically ill patients with sepsis require a multidisciplinary approach, as this situation implies multiorgan distress, with most of the bodily biochemical and cellular systems being affected by the condition. Moreover, sepsis is characterized by a multitude of biochemical interactions and by dynamic changes of the immune system. At the moment, there is a gap in our understanding of the cellular, genetic, and molecular mechanisms involved in sepsis.
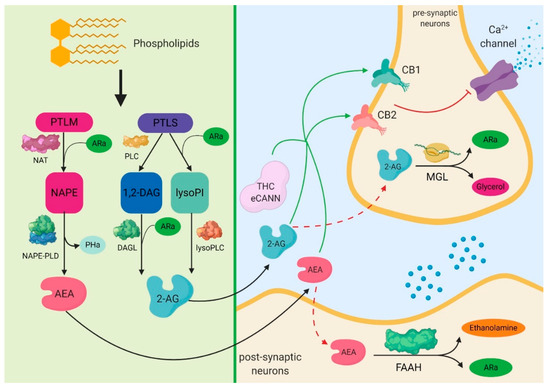
One of the systems intensely studied in recent years is the endocannabinoid signaling pathway, as light was shed over a series of important interactions of cannabinoid receptors with biochemical pathways, specifically for sepsis. Furthermore, a series of important implications on inflammation and the immune system that are induced by the activity of cannabinoid receptors stimulated by the delta-9-tetrahydrocannabinol (Δ9-THC) and cannabidiol (CBD) have been noticed.
One of the most important is their ability to reduce the biosynthesis of pro-inflammatory mediators and the modulation of immune mechanisms. Different studies have reported that cannabinoids can reduce oxidative stress at mitochondrial and cellular levels.
The aim of this review paper was to present, in detail, the important mechanisms modulated by the endocannabinoid signaling pathway, as well as of the molecular and cellular links it has with sepsis. At the same time, we wish to present the possible implications of cannabinoids in the most important biological pathways involved in sepsis, such as inflammation, redox activity, immune system, and epigenetic expression.”
https://www.ncbi.nlm.nih.gov/pubmed/32012914
https://www.mdpi.com/2073-4409/9/2/307

 “Uncontrolled infection and increased inflammatory mediators might cause systemic inflammatory response. It is already known that
“Uncontrolled infection and increased inflammatory mediators might cause systemic inflammatory response. It is already known that  “Sepsis is a life-threatening condition with high mortality rates that is caused by dysregulation of the host response to infection. We previously showed that treatment with the
“Sepsis is a life-threatening condition with high mortality rates that is caused by dysregulation of the host response to infection. We previously showed that treatment with the  “Sepsis is a clinical condition resulting from a dysregulated immune response to an infection that leads to organ dysfunction. Despite numerous efforts to optimize treatment, sepsis remains to be the main cause of death in most intensive care units.
The endogenous cannabinoid system (ECS) plays an important role in inflammation.
Cannabinoid receptor 2 (CB2R) activation is immunosuppressive, which might be beneficial during the hyper-inflammatory phase of sepsis.
Beta-caryophyllene (BCP) is a non-psychoactive natural cannabinoid (
“Sepsis is a clinical condition resulting from a dysregulated immune response to an infection that leads to organ dysfunction. Despite numerous efforts to optimize treatment, sepsis remains to be the main cause of death in most intensive care units.
The endogenous cannabinoid system (ECS) plays an important role in inflammation.
Cannabinoid receptor 2 (CB2R) activation is immunosuppressive, which might be beneficial during the hyper-inflammatory phase of sepsis.
Beta-caryophyllene (BCP) is a non-psychoactive natural cannabinoid ( “Sepsis is a clinical condition resulting from a dysregulated immune response to an infection that leads to organ dysfunction. Despite numerous efforts to optimize treatment, sepsis remains to be the main cause of death in most intensive care units.
The endogenous
“Sepsis is a clinical condition resulting from a dysregulated immune response to an infection that leads to organ dysfunction. Despite numerous efforts to optimize treatment, sepsis remains to be the main cause of death in most intensive care units.
The endogenous 
