 “Evidence on the use and efficacy of medical cannabis for children is limited. We examined clinical and epidemiological characteristics of medical cannabis treatment and caregiver-reported effects in children and adolescents in Switzerland.
“Evidence on the use and efficacy of medical cannabis for children is limited. We examined clinical and epidemiological characteristics of medical cannabis treatment and caregiver-reported effects in children and adolescents in Switzerland.
We collected clinical data from children and adolescents (< 18 years) who received Δ9-tetrahydrocannabinol (THC), cannabidiol (CBD), or a combination of the two between 2008 and 2019 in Switzerland. Out of 205 contacted families, 90 agreed to participate. The median age at the first prescription was 11.5 years (interquartile range (IQR) 6-16), and 32 patients were female (36%). Fifty-one (57%) patients received CBD only and 39 (43%) THC. Patients were more likely to receive THC therapy if one of the following symptoms or signs were present: spasticity, pain, lack of weight gain, vomiting, or nausea, whereas seizures were the dominant indication for CBD therapy.
Improvements were reported in 59 (66%) study participants.
The largest treatment effects were reported for pain, spasticity, and frequency of seizures in participants treated with THC, and for those treated with pure CBD, the frequency of seizures. However, 43% of caregivers reported treatment interruptions, mainly because of lack of improvement (56%), side effects (46%), the need for a gastric tube (44%), and cost considerations (23%).
Conclusions: The effects of medical cannabis in children and adolescents with chronic conditions are unknown except for rare seizure disorders, but the caregiver-reported data analysed here may justify trials of medical cannabis with standardized concentrations of THC or CBD to assess its efficacy in the young.
What is Known: • The use of medical cannabis (THC and CBD) to treat a variety of diseases among children and adolescents is increasing. • In contrast to adults, there is no evidence to support the use of medical cannabis to treat chronic pain and spasticity in children, but substantial evidence to support the use of CBD in children with rare seizure disorders.
What is New: • This study provides important insights into prescription practices, dosages, and treatment outcomes in children and adolescents using medical cannabis data from a real-life setting.
• The effects of medical cannabis in children and adolescents with chronic conditions shown in our study support trials of medical cannabis for chronic conditions.”
“For two thirds of participants treated with standardized THC or CBD preparations, the caregiver reported an improvement in their condition and well-being. Medical cannabis could be a promising and useful therapy for children and adolescents with neurological conditions.”
https://link.springer.com/article/10.1007%2Fs00431-021-04202-z

 “Ehlers-Danlos Syndromes (EDS) and related Hypermobility Spectrum Disorders (HSD) are debilitating connective tissue disorders that feature a prominent pain component for which there are limited therapeutic options for pain management.
“Ehlers-Danlos Syndromes (EDS) and related Hypermobility Spectrum Disorders (HSD) are debilitating connective tissue disorders that feature a prominent pain component for which there are limited therapeutic options for pain management.  “We present the case of an 18-year-old woman who suffered from complications of Ehlers-Danlos syndrome (EDS). Her pain was poorly controlled despite being on a myriad of analgesic medications at the time.
“We present the case of an 18-year-old woman who suffered from complications of Ehlers-Danlos syndrome (EDS). Her pain was poorly controlled despite being on a myriad of analgesic medications at the time. “In humans, various sites like cannabinoid receptors (CBR) having a binding affinity with cannabinoids are distributed on the surface of different cell types, where endocannabinoids (ECs) and derivatives of fatty acid can bind. The binding of these substance(s) triggers the activation of specific receptors required for various physiological functions, including pain sensation, memory, and appetite.
“In humans, various sites like cannabinoid receptors (CBR) having a binding affinity with cannabinoids are distributed on the surface of different cell types, where endocannabinoids (ECs) and derivatives of fatty acid can bind. The binding of these substance(s) triggers the activation of specific receptors required for various physiological functions, including pain sensation, memory, and appetite. 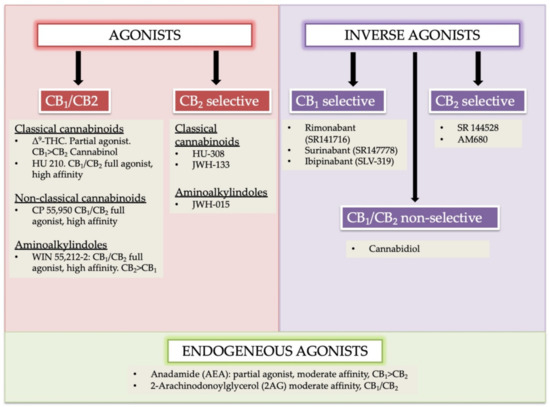
 “Chronic inflammation is considered to be a silent killer because it is the underlying cause of a wide range of clinical disorders, from cardiovascular to neurological diseases, and from cancer to obesity. In addition, there are over 80 different types of debilitating autoimmune diseases for which there are no cure. Currently, the drugs that are available to suppress chronic inflammation are either ineffective or overtly suppress the inflammation, thereby causing increased susceptibility to infections and cancer. Thus, the development of a new class of drugs that can suppress chronic inflammation is imperative.
“Chronic inflammation is considered to be a silent killer because it is the underlying cause of a wide range of clinical disorders, from cardiovascular to neurological diseases, and from cancer to obesity. In addition, there are over 80 different types of debilitating autoimmune diseases for which there are no cure. Currently, the drugs that are available to suppress chronic inflammation are either ineffective or overtly suppress the inflammation, thereby causing increased susceptibility to infections and cancer. Thus, the development of a new class of drugs that can suppress chronic inflammation is imperative. 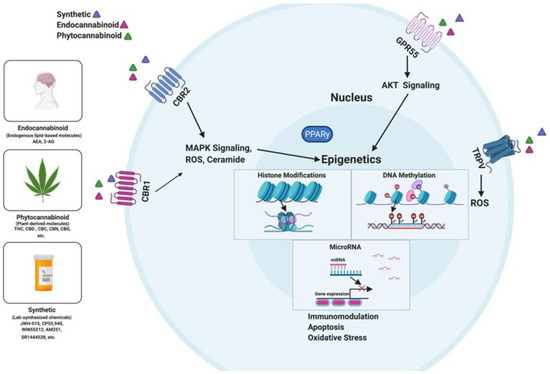
 “Central pain after stroke due to brainstem infarction is very rare. Treatment is difficult and specific guidelines are lacking. This is the report of a 61-year-old female patient who, after a posterolateral left medulla oblongata insult with incomplete Wallenberg syndrome, subsequently developed a burning and tingling pain in the contralateral leg and a burning and shooting pain in the ipsilateral face in trigeminal branches 1 and 2. More than 3 years of therapy with amitriptyline, gabapentin, pregabalin and various grade II and III opioids was ineffective or showed intolerable side effects. The administration of tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio improved the pain situation and quality of life quickly and permanently. The encouraging results in the present case may suggest that treatment with medical cannabis should be considered in similar cases when standard therapies are insufficient.”
“Central pain after stroke due to brainstem infarction is very rare. Treatment is difficult and specific guidelines are lacking. This is the report of a 61-year-old female patient who, after a posterolateral left medulla oblongata insult with incomplete Wallenberg syndrome, subsequently developed a burning and tingling pain in the contralateral leg and a burning and shooting pain in the ipsilateral face in trigeminal branches 1 and 2. More than 3 years of therapy with amitriptyline, gabapentin, pregabalin and various grade II and III opioids was ineffective or showed intolerable side effects. The administration of tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio improved the pain situation and quality of life quickly and permanently. The encouraging results in the present case may suggest that treatment with medical cannabis should be considered in similar cases when standard therapies are insufficient.”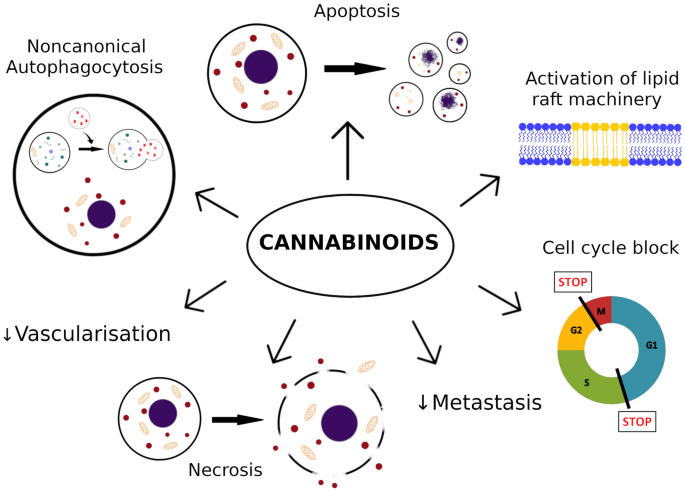
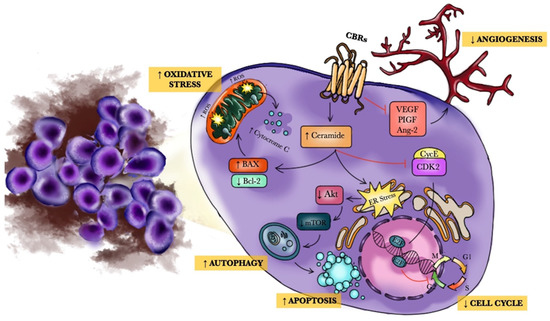
 “Medical marijuana (MM) use is common among cancer patients, but relatively little is known about the usage patterns and efficacy of MM used by gynecologic cancer patients.
“Medical marijuana (MM) use is common among cancer patients, but relatively little is known about the usage patterns and efficacy of MM used by gynecologic cancer patients. “
“