“CANNABIS may help to reduce brain damage after a stroke, new research suggests.
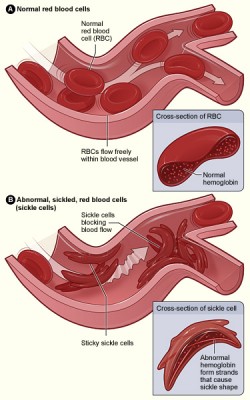
Chemical compounds found in the plant could help shrink the area of the brain affected by stroke, the study says.
Cannabinoids in the plant, as well as those that can be made artificially and those found naturally in the body, can also help improve brain function after a stroke attack, the authors said.
The study, which is to be presented to the annual UK Stroke Forum, examined previous studies conducted on the effect of the compound.
The authors, from the University of Nottingham, examined 94 studies evaluating the effects of cannabinoids on 1022 male rats, mice or monkeys.
They say the chemical “shows promise as a neuroprotective treatment for stroke”.
“This meta-analysis of pre-clinical stroke studies provides valuable information on the existing, and importantly, missing data on the use of cannabinoids as a potential treatment for stroke patients,” said lead author Dr Tim England, honorary consultant stroke physician at the University of Nottingham and Royal Derby Hospital.
Dr Dale Webb, director of research and information at the Stroke Association, added: “Stroke is the leading cause of adult disability in the UK, with more than half of all stroke survivors left dependent on others for everyday activities. With more people in the UK surviving a stroke, it’s never been more important to find new treatments to help more stroke patients make better recoveries.
“This new research is an example of the many new developments in the field of stroke which are being presented at this year’s UK Stroke Forum.
“The findings have identified the potential for cannabinoids to reduce brain damage caused by stroke.”