 “To assess any clinical improvement attributable to the addition of medical cannabis treatment (MCT) to the stable (>3 months) standard analgesic treatment of fibromyalgia (FM) patients, the retention rate and any changes in the concomitant analgesic treatment over a period of six months.
“To assess any clinical improvement attributable to the addition of medical cannabis treatment (MCT) to the stable (>3 months) standard analgesic treatment of fibromyalgia (FM) patients, the retention rate and any changes in the concomitant analgesic treatment over a period of six months.
METHODS:
The study involved 102 consecutive FM patients with VAS scores ≥4 despite standard analgesic treatment. Patients were prescribed two oil-diluted cannabis extracts: Bedrocan (22% THC, <1% CBD), and Bediol (6.3% THC, 8% CBD). FM severity was periodically assessed using Fibromyalgia Impact Questionnaire (FIQR), Fibromyalgia Assessment Scale (FAS), FACIT-Fatigue score, Pittsburgh Sleep Quality Index (PSQI), and Zung Depression and Anxiety Scales. During the study, patients were allowed to reduce or stop their concomitant analgesic therapy.
RESULTS:
The 6-month retention rate was 64%. A significant improvement in the PSQI and FIQR was observed in respectively 44% and 33% of patients. 50% showed a moderate improvement in the anxiety and depression scales. Multiple regression analysis showed a correlation between the body mass index (BMI) and FIQR improvement (p=0.017). Concomitant analgesic treatment was reduced or suspended in 47% of the patients. One-third experienced mild adverse events, which did not cause any significant treatment modifications.
CONCLUSIONS:
This observational study shows that adjunctive MCT offers a possible clinical advantage in FM patients, especially in those with sleep dysfunctions. The clinical improvement inversely correlated with BMI. The retention rate and changes in concomitant analgesic therapy reflect MCT efficacy of the improved quality of life of patients. Further studies are needed to confirm these data, identify MCT-responsive sub-groups of FM patients, and establish the most appropriate posology and duration of the therapy.”

 “While medical and recreational cannabis use is becoming more frequent among older adults, the neurocognitive consequences of cannabis use in this age group are unclear. The aim of this literature review was to synthesize and evaluate the current knowledge on the association of cannabis use during older-adulthood with cognitive function and brain aging.
“While medical and recreational cannabis use is becoming more frequent among older adults, the neurocognitive consequences of cannabis use in this age group are unclear. The aim of this literature review was to synthesize and evaluate the current knowledge on the association of cannabis use during older-adulthood with cognitive function and brain aging. “Microglia, the resident immune cells of the central nervous system, mediate brain homeostasis by controlling neuronal proliferation/differentiation and synaptic activity. In response to external signals from neuropathological conditions, homeostatic (M0) microglia can adopt one of two activation states: the classical (M1) activation state, which secretes mediators of the proinflammatory response, and the alternative (M2) activation state, which presumably mediates the resolution of neuroinflammation and tissue repair/remodeling.
“Microglia, the resident immune cells of the central nervous system, mediate brain homeostasis by controlling neuronal proliferation/differentiation and synaptic activity. In response to external signals from neuropathological conditions, homeostatic (M0) microglia can adopt one of two activation states: the classical (M1) activation state, which secretes mediators of the proinflammatory response, and the alternative (M2) activation state, which presumably mediates the resolution of neuroinflammation and tissue repair/remodeling.
 “Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
“Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).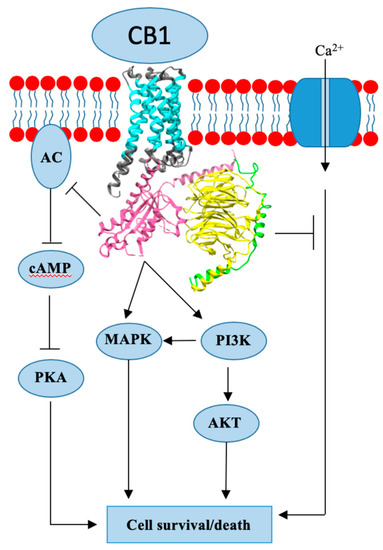
 “Clinical evidence supports effectiveness of
“Clinical evidence supports effectiveness of  “Alzheimer’s disease (AD) is characterized by progressive cognitive decline and pathologically by the accumulation of amyloid-β (Aβ) and tau hyperphosphorylation causing neurodegeneration and neuroinflammation. Current AD treatments do not stop or reverse the disease progression, highlighting the need for more effective therapeutics.
“Alzheimer’s disease (AD) is characterized by progressive cognitive decline and pathologically by the accumulation of amyloid-β (Aβ) and tau hyperphosphorylation causing neurodegeneration and neuroinflammation. Current AD treatments do not stop or reverse the disease progression, highlighting the need for more effective therapeutics. “Herein, 11 general types of natural cannabinoids from Cannabis sativa as well as 50 (-)-CBD analogues with therapeutic potential were described. The underlying molecular mechanisms of CBD as a therapeutic candidate for epilepsy and neurodegenerative diseases were comprehensively clarified. CBD indirectly acts as an endogenous cannabinoid receptor agonist to exert its neuroprotective effects. CBD also promotes neuroprotection through different signal transduction pathways mediated indirectly by cannabinoid receptors. Furthermore, CBD prevents the glycogen synthase kinase 3β (GSK-3β) hyperphosphorylation caused by Aβ and may be developed as a new therapeutic candidate for Alzheimer’s disease.”
“Herein, 11 general types of natural cannabinoids from Cannabis sativa as well as 50 (-)-CBD analogues with therapeutic potential were described. The underlying molecular mechanisms of CBD as a therapeutic candidate for epilepsy and neurodegenerative diseases were comprehensively clarified. CBD indirectly acts as an endogenous cannabinoid receptor agonist to exert its neuroprotective effects. CBD also promotes neuroprotection through different signal transduction pathways mediated indirectly by cannabinoid receptors. Furthermore, CBD prevents the glycogen synthase kinase 3β (GSK-3β) hyperphosphorylation caused by Aβ and may be developed as a new therapeutic candidate for Alzheimer’s disease.”
 “The 20% prevalence of chronic pain in the general population is a major health concern given the often profound associated impairment of daily activities, employment status, and health-related quality of life in sufferers. Resource utilization associated with chronic pain represents an enormous burden for healthcare systems. Although analgesia based on the World Health Organization’s pain ladder continues to be the mainstay of chronic pain management, aside from chronic cancer pain or end-of-life care, prolonged use of non-steroidal anti-inflammatory drugs or opioids to manage chronic pain is rarely sustainable.
“The 20% prevalence of chronic pain in the general population is a major health concern given the often profound associated impairment of daily activities, employment status, and health-related quality of life in sufferers. Resource utilization associated with chronic pain represents an enormous burden for healthcare systems. Although analgesia based on the World Health Organization’s pain ladder continues to be the mainstay of chronic pain management, aside from chronic cancer pain or end-of-life care, prolonged use of non-steroidal anti-inflammatory drugs or opioids to manage chronic pain is rarely sustainable.