 “The global cancer burden is significantly increasing at an alarming rate affecting patients, relatives, communities, and health-care system. Cancer patients require adequate pain relief and palliative care throughout the life course, especially in terminal illness. Although opioid treatment is successful in majority of patients, around 40% do not achieve enough analgesia or are prone to serious side effects and toxicity. The treatment of medical conditions with cannabis and cannabinoid compounds is constantly expanding. This review organizes the current knowledge in the context of SNPs associated with opioids and nonopioids and its clinical consequences in pain management and pharmacogenetic targets of cannabinoids, for use in clinical practice.”
“The global cancer burden is significantly increasing at an alarming rate affecting patients, relatives, communities, and health-care system. Cancer patients require adequate pain relief and palliative care throughout the life course, especially in terminal illness. Although opioid treatment is successful in majority of patients, around 40% do not achieve enough analgesia or are prone to serious side effects and toxicity. The treatment of medical conditions with cannabis and cannabinoid compounds is constantly expanding. This review organizes the current knowledge in the context of SNPs associated with opioids and nonopioids and its clinical consequences in pain management and pharmacogenetic targets of cannabinoids, for use in clinical practice.”
Category Archives: Cancer
Hempseed Lignanamides Rich-Fraction: Chemical Investigation and Cytotoxicity towards U-87 Glioblastoma Cells.
 “The weak but noteworthy presence of (poly)phenols in hemp seeds has been long overshadowed by the essential polyunsaturated fatty acids and digestible proteins, considered responsible for their high nutritional benefits. Instead, lignanamides and their biosynthetic precursors, phenylamides, seem to display interesting and diverse biological activities only partially clarified in the last decades. Herein, negative mode HR-MS/MS techniques were applied to the chemical investigation of a (poly)phenol-rich fraction, obtained from hemp seeds after extraction/fractionation steps. This extract contained phenylpropanoid amides and their random oxidative coupling derivatives, lignanamides, which were the most abundant compounds and showed a high chemical diversity, deeply unraveled through high resolution tandem mass spectrometry (HR-MS/MS) tools.
“The weak but noteworthy presence of (poly)phenols in hemp seeds has been long overshadowed by the essential polyunsaturated fatty acids and digestible proteins, considered responsible for their high nutritional benefits. Instead, lignanamides and their biosynthetic precursors, phenylamides, seem to display interesting and diverse biological activities only partially clarified in the last decades. Herein, negative mode HR-MS/MS techniques were applied to the chemical investigation of a (poly)phenol-rich fraction, obtained from hemp seeds after extraction/fractionation steps. This extract contained phenylpropanoid amides and their random oxidative coupling derivatives, lignanamides, which were the most abundant compounds and showed a high chemical diversity, deeply unraveled through high resolution tandem mass spectrometry (HR-MS/MS) tools.
The effect of different doses of the lignanamides-rich extract (LnHS) on U-87 glioblastoma cell line and non-tumorigenic human fibroblasts was evaluated. Thus, cell proliferation, genomic DNA damage, colony forming and wound repair capabilities were assessed, as well as LnHS outcome on the expression levels of pro-inflammatory cytokines. LnHS significantly inhibited U-87 cancer cell proliferation, but not that of fibroblasts, and was able to reduce U-87 cell migration, inducing further DNA damage. No modification in cytokines’ expression level was found. Data acquired suggested that LnHS acted in U-87 cells by inducing the apoptosis machinery and suppressing the autophagic cell death.”
Insight of Druggable Cannabinoids against Estrogen Receptor β in Breast Cancer.

“Breast cancer (BC) is the second most prevalent cancer worldwide.
Estrogen receptor beta (ERβ) is an essential protein of breast cells to suppress estrogen induced uncontrolled proliferation. Thus small molecules that can modulate and enhance ERβ expression would be an effective agent to suppress BC development.
Studies showed that cannabinoid (CB), specifically Delta-9-tetrahydrocannabinol (Del9THC), can increase the expression of ERβ and inhibits BC cell proliferation.
In this study, less psychoactive and structurally similar analogues of Del9THC were chosen as drug candidates and ERβ was targeted as a therapeutic receptor. Delta-8-tetrahydrocannabinol (Del8THC) and Delta-4-Isotetrahydrocannabinol (Del4isoTHC) were the drug candidates selected on the basis of literature reports, Absorption, Distribution, Metabolism, Excretion and Toxicity (ADMET) properties, medicinal chemistry profile and physicochemical features.
Molecular docking simulations were carried out to determine ligand receptor interactions and binding affinity based on free binding energy. To get a better drug, the structural modification was done on Del8THC and generated a new CB analogue called Cannabinoid A.
Finally, molecular interaction analysis revealed that two CBs and one of their analogue interact with the active site residues of ERβ. Therefore, this study revealed a new way to discover novel drug(s) for BC patients.”
https://www.ncbi.nlm.nih.gov/pubmed/32116130
https://www.tandfonline.com/doi/abs/10.1080/07391102.2020.1737233?journalCode=tbsd20
Cannabinoids and Hormone Receptor-Positive Breast Cancer Treatment.
 “Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
“Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
Endogenous cannabinoids together with cannabinoid receptor 1 and 2 (CB1, CB2) constitute the basis of the endocannabinoid system.
Interactions of cannabinoids with hypothalamic-pituitary-gonadal axis hormones are well documented, and two studies found a positive correlation between peak plasma endogenous cannabinoid anandamide with peak plasma 17β-estradiol, luteinizing hormone and follicle-stimulating hormone levels at ovulation in healthy premenopausal women. Do cannabinoids have an effect on HR+ BC? In this paper we review known and possible interactions between cannabinoids and specific HR+ BC treatments.
In preclinical studies, CB1 and CB2 agonists (i.e., anandamide, THC) have been shown to inhibit the proliferation of ER positive BC cell lines.
There is less evidence for antitumor cannabinoid action in HR+ BC in animal models and there are no clinical trials exploring the effects of cannabinoids on HR+ BC treatment outcomes. Two studies have shown that tamoxifen and several other selective estrogen receptor modulators (SERM) can act as inverse agonists on CB1 and CB2, an interaction with possible clinical consequences. In addition, cannabinoid action could interact with other commonly used endocrine and targeted therapies used in the treatment of HR+ BC.”
https://www.ncbi.nlm.nih.gov/pubmed/32106399
https://www.mdpi.com/2072-6694/12/3/525
The Endocannabinoid System Alleviates Pain in a Murine Model of Cancer-Induced Bone Pain.
 “Metastatic breast cancer is prevalent worldwide, and one of the most common sites of metastasis are long bones. Of patients with disease, the major symptom is pain, yet current medications fail to adequately result in analgesic efficacy and present major undesirable adverse effects.
“Metastatic breast cancer is prevalent worldwide, and one of the most common sites of metastasis are long bones. Of patients with disease, the major symptom is pain, yet current medications fail to adequately result in analgesic efficacy and present major undesirable adverse effects.
In our study we investigate the potential of a novel monoacylglycerol lipase (MAGL) inhibitor, MJN110, in a murine model of cancer induced bone pain (CIBP). Literature has previously demonstrated that MAGL inhibitors function to increase the endogenous concentrations of 2-arachydonylglycerol, which then activate CB1 and CB2 receptors inhibiting inflammation and pain.
Together, these data support the application for MJN110 as a novel therapeutic for cancer induced bone pain.
SIGNIFICANCE STATEMENT: Current standard of care for metastatic breast cancer pain is opioid-based therapies with adjunctive chemotherapy, which have highly addictive and other deleterious side effects. The need for effective, non-opioid based therapies is essential and harnessing the endogenous cannabinoid system is proving to be a new target to treat various types of pain conditions. We present a novel drug targeting the endogenous cannabinoid system that is effective at reducing pain in a mouse model of metastatic breast cancer to bone.”
https://www.ncbi.nlm.nih.gov/pubmed/32054717
http://jpet.aspetjournals.org/content/early/2020/02/13/jpet.119.262337
Inhibition of autophagic flux differently modulates cannabidiol-induced death in 2D and 3D glioblastoma cell cultures.

There is some evidence that cannabidiol (CBD) can induce cell death and increases the radiosensitivity of GBM by enhancing apoptosis. Beside initiation of death, CBD has been demonstrated as an inducer of autophagy.
In the present study, we address the question whether CBD simultaneously induces a protective effect in GBM by upregulating autophagy. Addition of chloroquine that suppressed autophagic flux to 2D GBM cultures increased CBD-induced cell death, presenting proof for the protective autophagy.
Blockage of autophagy upregulated radiation-induced cytotoxicity but only modestly affected the levels of cell death in CBD- or CBD/γ-irradiated 3D GBM cultures. Furthermore, CBD enhanced the pro-apoptotic activities of JNK1/2 and MAPK p38 signaling cascades while partially downregulated the pro-survival PI3K-AKT cascade, thereby changing a balance between cell death and survival.
Suppression of JNK activation partially reduced CBD-induced cell death in 3D GBM cultures. In contrast, co-treatment of CBD-targeted cells with inhibitors of PI3K-AKT-NF-κB, IKK-NF-κB or JAK2-STAT3 pathways killed surviving GBM cells in both 2D and 3D cultures, potentially improving the therapeutic ratio of GBM.”
https://www.ncbi.nlm.nih.gov/pubmed/32060308
“Killing efficiency of cannabinoids (CBD, THC and their combination CBD+THC) against GBM in vitro and in animal experiments has been elucidated in numerous studies during the last 15 years. Additional investigations also confirmed a cytotoxic role of cannabinoids for several other types of cancer. A number of studies demonstrated the efficiency of combined treatments of cannabinoids together with γ-irradiation in both cell culture and in animal experiments.”
Cannabinoid receptor expression in non-small cell lung cancer. Effectiveness of tetrahydrocannabinol and cannabidiol inhibiting cell proliferation and epithelial-mesenchymal transition in vitro.
 “Patients with non-small cell lung cancer (NSCLC) develop resistance to antitumor agents by mechanisms that involve the epithelial-to-mesenchymal transition (EMT). This necessitates the development of new complementary drugs, e.g., cannabinoid receptors (CB1 and CB2) agonists including tetrahydrocannabinol (THC) and cannabidiol (CBD).
“Patients with non-small cell lung cancer (NSCLC) develop resistance to antitumor agents by mechanisms that involve the epithelial-to-mesenchymal transition (EMT). This necessitates the development of new complementary drugs, e.g., cannabinoid receptors (CB1 and CB2) agonists including tetrahydrocannabinol (THC) and cannabidiol (CBD).
The combined use of THC and CBD confers greater benefits, as CBD enhances the effects of THC and reduces its psychotropic activity. We assessed the relationship between the expression levels of CB1 and CB2 to the clinical features of a cohort of patients with NSCLC, and the effect of THC and CBD (individually and in combination) on proliferation, EMT and migration in vitro in A549, H460 and H1792 lung cancer cell lines.
METHODS:
Expression levels of CB1, CB2, EGFR, CDH1, CDH2 and VIM were evaluated by quantitative reverse transcription-polymerase chain reaction. THC and CBD (10-100 μM), individually or in combination (1:1 ratio), were used for in vitro assays. Cell proliferation was determined by BrdU incorporation assay. Morphological changes in the cells were visualized by phase-contrast and fluorescence microscopy. Migration was studied by scratch recolonization induced by 20 ng/ml epidermal growth factor (EGF).
RESULTS:
The tumor samples were classified according to the level of expression of CB1, CB2, or both. Patients with high expression levels of CB1, CB2, and CB1/CB2 showed increased survival reaching significance for CB1 and CB1/CB2 (p = 0.035 and 0.025, respectively).
Both cannabinoid agonists inhibited the proliferation and expression of EGFR in lung cancer cells, and CBD potentiated the effect of THC. THC and CBD alone or in combination restored the epithelial phenotype, as evidenced by increased expression of CDH1 and reduced expression of CDH2 and VIM, as well as by fluorescence analysis of cellular cytoskeleton.
Finally, both cannabinoids reduced the in vitro migration of the three lung cancer cells lines used.
CONCLUSIONS:
The expression levels of CB1 and CB2 have a potential use as markers of survival in patients with NSCLC. THC and CBD inhibited the proliferation and expression of EGFR in the lung cancer cells studied. Finally, the THC/CBD combination restored the epithelial phenotype in vitro.”
https://www.ncbi.nlm.nih.gov/pubmed/32049991
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0228909
Targeting GPCRs Against Cardiotoxicity Induced by Anticancer Treatments.
 “Novel anticancer medicines, including targeted therapies and immune checkpoint inhibitors, have greatly improved the management of cancers. However, both conventional and new anticancer treatments induce cardiac adverse effects, which remain a critical issue in clinic.
“Novel anticancer medicines, including targeted therapies and immune checkpoint inhibitors, have greatly improved the management of cancers. However, both conventional and new anticancer treatments induce cardiac adverse effects, which remain a critical issue in clinic.
Cardiotoxicity induced by anti-cancer treatments compromise vasospastic and thromboembolic ischemia, dysrhythmia, hypertension, myocarditis, and cardiac dysfunction that can result in heart failure. Importantly, none of the strategies to prevent cardiotoxicity from anticancer therapies is completely safe and satisfactory.
Certain clinically used cardioprotective drugs can even contribute to cancer induction. Since G protein coupled receptors (GPCRs) are target of forty percent of clinically used drugs, here we discuss the newly identified cardioprotective agents that bind GPCRs of adrenalin, adenosine, melatonin, ghrelin, galanin, apelin, prokineticin and cannabidiol.
We hope to provoke further drug development studies considering these GPCRs as potential targets to be translated to treatment of human heart failure induced by anticancer drugs.”
https://www.ncbi.nlm.nih.gov/pubmed/32039239
https://www.frontiersin.org/articles/10.3389/fcvm.2019.00194/full
“Cannabidiol Protects against Doxorubicin-Induced Cardiomyopathy by Modulating Mitochondrial Function and Biogenesis.” https://www.ncbi.nlm.nih.gov/pubmed/25569804
Cannabinoid Signaling in Glioma Cells.
 “Cannabinoids are a group of structurally heterogeneous but pharmacologically related compounds, including plant-derived cannabinoids, synthetic substances and endogenous cannabinoids, such as anandamide and 2-arachidonoylglycerol.
“Cannabinoids are a group of structurally heterogeneous but pharmacologically related compounds, including plant-derived cannabinoids, synthetic substances and endogenous cannabinoids, such as anandamide and 2-arachidonoylglycerol.
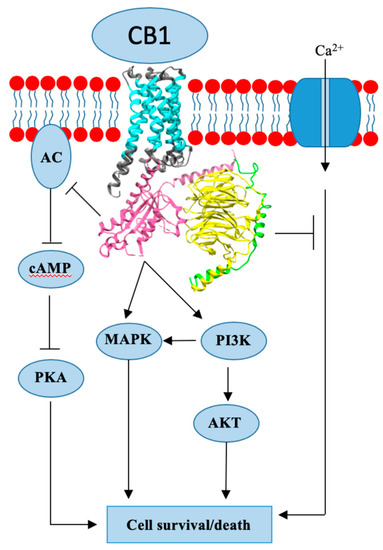
Cannabinoids elicit a wide range of central and peripheral effects mostly mediated through cannabinoid receptors. There are two types of specific Gi/o-protein-coupled receptors cloned so far, called CB1 and CB2, although an existence of additional cannabinoid-binding receptors has been suggested. CB1 and CB2 differ in their predicted amino acid sequence, tissue distribution, physiological role and signaling mechanisms.
Significant alterations of a balance in the cannabinoid system between the levels of endogenous ligands and their receptors occur during malignant transformation in various types of cancer, including gliomas.
Cannabinoids exert anti-proliferative action in tumor cells.
Induction of cell death by cannabinoid treatment relies on the generation of a pro-apoptotic sphingolipid ceramide and disruption of signaling pathways crucial for regulation of cellular proliferation, differentiation or apoptosis. Increased ceramide levels lead also to ER-stress and autophagy in drug-treated glioblastoma cells.
Beyond blocking of tumor cells proliferation cannabinoids inhibit invasiveness, angiogenesis and the stem cell-like properties of glioma cells, showing profound activity in the complex tumor microenvironment. Advances in translational research on cannabinoid signaling led to clinical investigations on the use of cannabinoids in treatments of glioblastomas.”
https://www.ncbi.nlm.nih.gov/pubmed/32034716
https://link.springer.com/chapter/10.1007%2F978-3-030-30651-9_11
“Cannabinoids exert anti-proliferative action in tumor cells.” https://www.ncbi.nlm.nih.gov/pubmed/22879071
“A glioma is a primary brain tumor that originates from the supportive cells of the brain, called glial cells.” http://neurosurgery.ucla.edu/body.cfm?id=159
“Remarkably, cannabinoids kill glioma cells selectively and can protect non-transformed glial cells from death.” http://www.ncbi.nlm.nih.gov/pubmed/15275820
The Highs and Lows of Cannabis in Cancer Treatment and Bone Marrow Transplantation.
 “In the last decade, we have observed an increased public and scientific interest in the clinical applications of medical cannabis.
“In the last decade, we have observed an increased public and scientific interest in the clinical applications of medical cannabis.
Currently, the application of cannabinoids in cancer patients is mainly due to their analgesic and anti-emetic effects.
The direct effects of phyto-cannabinoids on cancer cells are under intensive research, and the data remain somewhat inconsistent. Although anti-proliferative properties were observed in vitro, conclusive data from animal models and clinical trials are lacking.
Since immunotherapy of malignant diseases and bone marrow transplantation are integral approaches in hemato-oncology, the immuno-modulatory characteristic of cannabinoids is a fundamental aspect for consideration. The effect of cannabinoids on the immune system is presently under investigation, and some evidence for its immuno-regulatory properties has been shown.
In addition, the interaction of cannabinoids and classical cytotoxic agents is a subject for further investigation. Here we discuss the current knowledge of cannabinoid-based treatments in preclinical models and the limited data in oncological patients. Particularly, we address the possible contradiction between the direct anti-tumor and the immune-modulatory effects of cannabinoids.
Better understanding of the mechanism of cannabinoids influence is essential to design therapies that will allow cannabinoids to be incorporated into the clinic.”
