 “Opioid receptor agonist drugs, such as morphine, are very effective for treating chronic and severe pain; but, tolerance can develop with long-term use. Although there is a lot of information about the pathophysiological mechanisms of opioid tolerance, it is still not fully clarified. Suggested mechanisms for opioid tolerance include opioid receptor desensitisation, reduction of sensitivity G-proteins, activation of mitogen-activated protein kinase (MAPK), altered intracellular signaling pathway including nitric oxide, and activation of mammalian target of rapamycin (mTOR).
“Opioid receptor agonist drugs, such as morphine, are very effective for treating chronic and severe pain; but, tolerance can develop with long-term use. Although there is a lot of information about the pathophysiological mechanisms of opioid tolerance, it is still not fully clarified. Suggested mechanisms for opioid tolerance include opioid receptor desensitisation, reduction of sensitivity G-proteins, activation of mitogen-activated protein kinase (MAPK), altered intracellular signaling pathway including nitric oxide, and activation of mammalian target of rapamycin (mTOR).
One way to reduce opioid tolerance and increase the analgesic potential is to use low doses. Combination of cannabinoids with opioids has been shown to manifest reduce the opioid dose. Experimental studies revealed an interaction of the endocannabinoid system and opioid antinociception.
Cannabinoid and opioid receptor systems use common pathways in the formation of analgesic effect and demonstrate their activity via G protein coupled receptors (GPCR). Cannabinoid drugs modulate opioid analgesic activity at a number of distinct levels within the cell, ranging from direct receptor associations, to post-receptor interactions through shared signal transduction pathways.
This review summarizes the data indicating that with combining cannabinoids and opioids drugs may be able to produce long-term analgesic effects, while preventing the opioid analgesic tolerance.”

 “Excessive fear and anxiety, coupled with corticolimbic dysfunction, are core features of stress- and trauma-related psychopathology, such as posttraumatic stress disorder (PTSD).
“Excessive fear and anxiety, coupled with corticolimbic dysfunction, are core features of stress- and trauma-related psychopathology, such as posttraumatic stress disorder (PTSD). “Endocannabinoids play important roles in regulating CNS synaptic function and peripheral metabolism, but
“Endocannabinoids play important roles in regulating CNS synaptic function and peripheral metabolism, but  “Generally, the development and progression of neurodegenerative diseases are associated with advancing age, so they are usually diagnosed in late adulthood. A primary mechanism underlying the onset of neurodegenerative diseases is neuroinflammation. Based on this background, the concept of “neuroinflammaging” has emerged. In this deregulated neuroinflammatory process, a variety of immune cells participate, especially glial cells, proinflammatory cytokines, receptors, and subcellular organelles including mitochondria, which are mainly responsible for maintaining redox balance at the cellular level. Senescence and autophagic processes also play a crucial role in the neuroinflammatory disease associated with aging.
“Generally, the development and progression of neurodegenerative diseases are associated with advancing age, so they are usually diagnosed in late adulthood. A primary mechanism underlying the onset of neurodegenerative diseases is neuroinflammation. Based on this background, the concept of “neuroinflammaging” has emerged. In this deregulated neuroinflammatory process, a variety of immune cells participate, especially glial cells, proinflammatory cytokines, receptors, and subcellular organelles including mitochondria, which are mainly responsible for maintaining redox balance at the cellular level. Senescence and autophagic processes also play a crucial role in the neuroinflammatory disease associated with aging. “Cannabis use among inflammatory bowel disease (IBD) patients is common. There are many studies of various laboratory models demonstrating the anti-inflammatory effect of cannabis, but their translation to human disease is still lacking.
“Cannabis use among inflammatory bowel disease (IBD) patients is common. There are many studies of various laboratory models demonstrating the anti-inflammatory effect of cannabis, but their translation to human disease is still lacking. “Excessive activation of the sympatho-adrenomedullary system plays a pathogenic role in triggering and sustaining essential hypertension. We previously reported that, in normotensive rats, intracerebroventricularly (i.c.v.) administered neuropeptides, corticotropin-releasing factor and bombesin induced activation of the sympatho-adrenomedullary system, and that brain
“Excessive activation of the sympatho-adrenomedullary system plays a pathogenic role in triggering and sustaining essential hypertension. We previously reported that, in normotensive rats, intracerebroventricularly (i.c.v.) administered neuropeptides, corticotropin-releasing factor and bombesin induced activation of the sympatho-adrenomedullary system, and that brain  “For many centuries,
“For many centuries,  “Microglia, the resident immune cells of the central nervous system, mediate brain homeostasis by controlling neuronal proliferation/differentiation and synaptic activity. In response to external signals from neuropathological conditions, homeostatic (M0) microglia can adopt one of two activation states: the classical (M1) activation state, which secretes mediators of the proinflammatory response, and the alternative (M2) activation state, which presumably mediates the resolution of neuroinflammation and tissue repair/remodeling.
“Microglia, the resident immune cells of the central nervous system, mediate brain homeostasis by controlling neuronal proliferation/differentiation and synaptic activity. In response to external signals from neuropathological conditions, homeostatic (M0) microglia can adopt one of two activation states: the classical (M1) activation state, which secretes mediators of the proinflammatory response, and the alternative (M2) activation state, which presumably mediates the resolution of neuroinflammation and tissue repair/remodeling. “Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
“Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).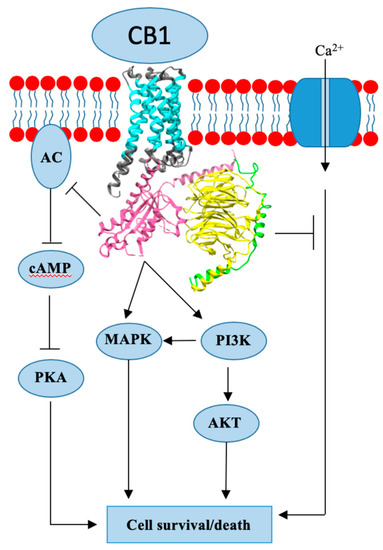
 “The 20% prevalence of chronic pain in the general population is a major health concern given the often profound associated impairment of daily activities, employment status, and health-related quality of life in sufferers. Resource utilization associated with chronic pain represents an enormous burden for healthcare systems. Although analgesia based on the World Health Organization’s pain ladder continues to be the mainstay of chronic pain management, aside from chronic cancer pain or end-of-life care, prolonged use of non-steroidal anti-inflammatory drugs or opioids to manage chronic pain is rarely sustainable.
“The 20% prevalence of chronic pain in the general population is a major health concern given the often profound associated impairment of daily activities, employment status, and health-related quality of life in sufferers. Resource utilization associated with chronic pain represents an enormous burden for healthcare systems. Although analgesia based on the World Health Organization’s pain ladder continues to be the mainstay of chronic pain management, aside from chronic cancer pain or end-of-life care, prolonged use of non-steroidal anti-inflammatory drugs or opioids to manage chronic pain is rarely sustainable.