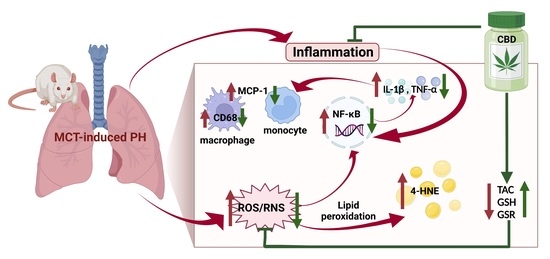
“Background: Cytokine release syndrome, also termed “cytokine storm,” is the leading cause of morbidity and mortality among patients with various conditions such as sepsis. While cytokine storm is associated with multiple organ damage, acute cardiac and renal injury represents a hallmark of cytokine storm. Since recent reports have suggested that cannabidiol (CBD) may assist in the treatment of inflammatory diseases, our objective was to examine the effect of CBD on cytokine storm-induced cardiac and renal injury using the lipopolysaccharide (LPS)-induced sepsis mouse model.
Materials and Methods: At 8 weeks of age, mice were randomly assigned to receive CBD (15 mg/kg) or vehicle one hour before a single injection of either phosphate-buffered saline or LPS (10 mg/kg) for an additional 24 h.
Results: Our results show that CBD improves cardiac function and reduces renal injury in a mouse model of cytokine storm. Moreover, our data indicate that CBD significantly reduces systemic and renal inflammation to contribute to the improvements observed in a cytokine storm-model of cardiac and renal injury.
Conclusions: Overall, the findings of this study suggest that CBD could be repurposed to reduce morbidity in patients with cytokine storm particularly in severe infections such as sepsis.”
https://pubmed.ncbi.nlm.nih.gov/36594988/
https://www.liebertpub.com/doi/10.1089/can.2022.0170