 “This study aims to determine the frequency of coronary artery disease among young to middle aged adults presenting with chest pain who currently use marijuana as compared to nonusers.
“This study aims to determine the frequency of coronary artery disease among young to middle aged adults presenting with chest pain who currently use marijuana as compared to nonusers.
Only 6.8% of the 146 marijuana users had evidence of coronary artery disease on coronary CT angiography. In comparison, the rate was 15.0% among the 1,274 marijuana nonusers.
A majority of marijuana users were younger than nonusers and had a lower frequency of hypertension and diabetes than nonusers.
There was no statistical difference in lipid panel values between the two groups.
CONCLUSION:
Among younger patients being evaluated for chest pain, self-reported cannabis use conferred no additional risk of coronary artery disease as detected on coronary CT angiography.”
https://www.ncbi.nlm.nih.gov/pubmed/31995626
“There is no association between marijuana use and the presence of coronary artery disease on coronary CT angiography in young to middle aged patients presenting with chest pain.”
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0228326

 “Endo-, phyto- and synthetic cannabinoids have been proposed as promising anti-cancer agents able to impair cancer cells’ behavior without affecting their non-transformed counterparts.
“Endo-, phyto- and synthetic cannabinoids have been proposed as promising anti-cancer agents able to impair cancer cells’ behavior without affecting their non-transformed counterparts.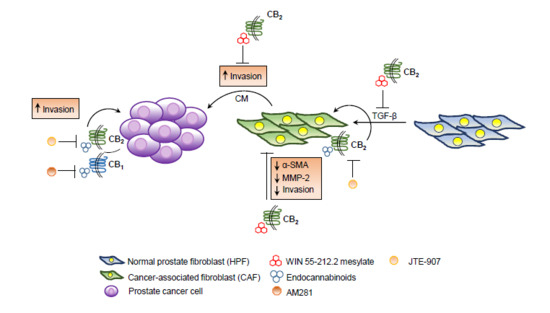
 “Recent evidence suggests that
“Recent evidence suggests that  “Medical marijuana is becoming widely available to patients in the U.S. and with recreational marijuana now legalized in many states, patient interest is on the rise.
“Medical marijuana is becoming widely available to patients in the U.S. and with recreational marijuana now legalized in many states, patient interest is on the rise. “Irritable bowel syndrome (IBS) global burden is underestimated despite its high prevalence. It’s a gastrointestinal disease having obscure pathophysiology with multiple therapies yet unsatisfactory remedies.
“Irritable bowel syndrome (IBS) global burden is underestimated despite its high prevalence. It’s a gastrointestinal disease having obscure pathophysiology with multiple therapies yet unsatisfactory remedies. “Palliative medicine physicians are challenged by lack of guidance regarding effectiveness and dosing of cannabis products in the setting of their emerging popularity.
“Palliative medicine physicians are challenged by lack of guidance regarding effectiveness and dosing of cannabis products in the setting of their emerging popularity. “Chronic neuropathic pain (NEP) is associated with growing therapeutic cannabis use. To promote quality of life without psychotropic effects, cannabinoids other than Δ9-tetrahydrocannabidiol, including
“Chronic neuropathic pain (NEP) is associated with growing therapeutic cannabis use. To promote quality of life without psychotropic effects, cannabinoids other than Δ9-tetrahydrocannabidiol, including  “Given the growing challenges in chronic pain management coupled with the ongoing consequences of the opioid epidemic, pain management practitioners are looking into more effective, innovative, and safer alternatives to treat pain.
“Given the growing challenges in chronic pain management coupled with the ongoing consequences of the opioid epidemic, pain management practitioners are looking into more effective, innovative, and safer alternatives to treat pain. “Abnormal
“Abnormal