“The use of cannabis, or marijuana, for medicinal purposes is deeply rooted though history, dating back to ancient times. It once held a prominent position in the history of medicine, recommended by many eminent physicians for numerous diseases, particularly headache and migraine.
Through the decades, this plant has taken a fascinating journey from a legal and frequently prescribed status to illegal, driven by political and social factors rather than by science.
However, with an abundance of growing support for its multitude of medicinal uses, the misguided stigma of cannabis is fading, and there has been a dramatic push for legalizing medicinal cannabis and research.
Almost half of the United States has now legalized medicinal cannabis, several states have legalized recreational use, and others have legalized cannabidiol-only use, which is one of many therapeutic cannabinoids extracted from cannabis.
Physicians need to be educated on the history, pharmacology, clinical indications, and proper clinical use of cannabis, as patients will inevitably inquire about it for many diseases, including chronic pain and headache disorders for which there is some intriguing supportive evidence…
The literature suggests that the medicinal use of cannabis may have a therapeutic role for a multitude of diseases, particularly chronic pain disorders including headache.
Supporting literature suggests a role for medicinal cannabis and cannabinoids in several types of headache disorders including migraine and cluster headache, although it is primarily limited to case based, anecdotal, or laboratory-based scientific research.
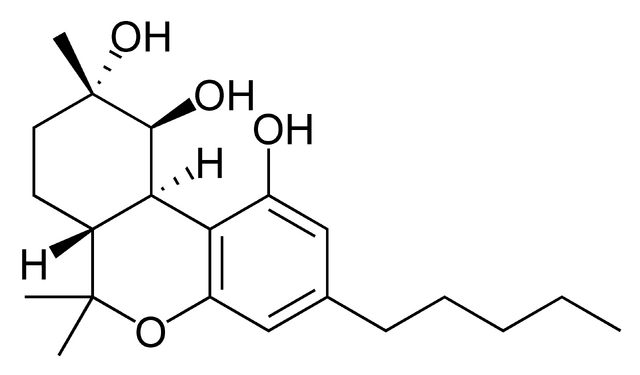
Cannabis contains an extensive number of pharmacological and biochemical compounds, of which only a minority are understood, so many potential therapeutic uses likely remain undiscovered.
Cannabinoids appear to modulate and interact at many pathways inherent to migraine, triptan mechanisms ofaction, and opiate pathways, suggesting potential synergistic or similar benefits.
Modulation of the endocannabinoid system through agonism or antagonism of its receptors, targeting its metabolic pathways, or combining cannabinoids with other analgesics for synergistic effects, may provide the foundation for many new classes of medications.”
http://www.ncbi.nlm.nih.gov/pubmed/26015168
http://www.thctotalhealthcare.com/category/headachemigraine/