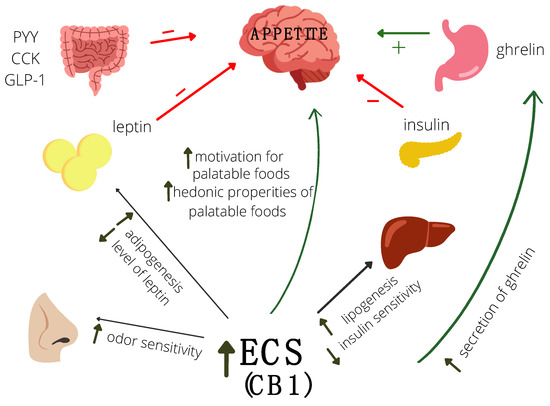
“This systematic review examine the biological effects of CBD, a major component of therapeutic Cannabis, on human pathological and cancer cell populations of integumentary, gastro-intestinal, genital and breast, respiratory, nervous, haematopoietic and skeletal districts in terms of cell viability, proliferation, migration, apoptosis, inflammation, metastasis, and CBD receptor expression. The included studies were in English, on human cell lines and primary culture from non-healthy donors with CBD exposure as variable and no CBD exposure as control. Quality assessment was based on ToxRtool with a reliability score ranging from 15 to 18. Following the PRISMA statement 4 independent reviewers performed an electronic search using MEDLINE via PubMed, Scopus and Web of Science. From 3974 articles, 83 studies have been selected. Data showed conflicting results due to different concentration exposure, administrations and time points. CBD inhibited cell viability and proliferation in most cellular districts except the integumentary apparatus. Also a significant inhibition of migration was observed in all cell types, while an increase in apoptosis at both high and low doses (greater and less than 10μM respectively). Considering inflammation, CBD caused an anti-inflammatory effect on nervous cells at low doses and on gastro-intestinal cells at high doses, while metastatic power was reduced even at low doses, but in a skeletal cell line there was an increased angiogenesis. CB1 receptor has been related to viability effects, CB2 to apoptosis and TRPV1 to inflammation and invasiveness. A detailed insight into these aspects would allow therapeutic use of this substance without possible side effects.”
https://pubmed.ncbi.nlm.nih.gov/35643249/
https://www.sciencedirect.com/science/article/abs/pii/S1043661822002122?via%3Dihub