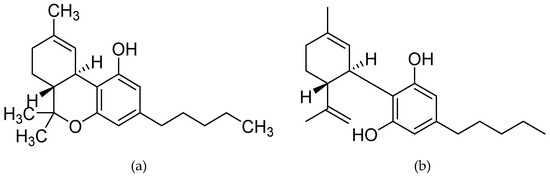
 “Many people with MS (pwMS) use unregulated cannabis or cannabis products to treat the symptoms associated with the disease. In line with this, Sativex, a synthetic combination of cannabidiol (CBD) and Δ9-tetrahydrocannabinol (Δ9-THC) has been approved to treat symptoms of spasticity.
“Many people with MS (pwMS) use unregulated cannabis or cannabis products to treat the symptoms associated with the disease. In line with this, Sativex, a synthetic combination of cannabidiol (CBD) and Δ9-tetrahydrocannabinol (Δ9-THC) has been approved to treat symptoms of spasticity.
In animals, CBD is effective in reducing the amounts of T-cell infiltrates in the spinal cord, suggesting CBD has anti-inflammatory properties. By doing this, CBD has shown to delay symptom onset in animal models of multiple sclerosis and slow disease progression. Importantly, combinations of CBD and Δ9-THC appear more effective in treating animal models of multiple sclerosis.
While CBD reduces the amounts of cell infiltrates in the spinal cord, Δ9-THC reduces scores of spasticity. In human studies, the results are less encouraging and conflict with the findings in animals. Drugs which deliver a combination of Δ9-THC and CBD in a 1:1 ratio appear to be only moderately effective in reducing spasticity scores, but appear to be almost as effective as current front-line treatments and cause less severe side effects than other treatments, such as baclofen (a GABA-B receptor agonist) and tizanidine (an α2 adrenergic receptor agonist).
The findings of the studies reviewed suggest that cannabinoids may help treat neuropathic pain in pwMS as an add-on therapy to already established pain treatments.
Long term double-blind placebo studies are greatly needed to further our understanding of the role of cannabinoids in multiple sclerosis treatment.”
https://pubmed.ncbi.nlm.nih.gov/33113776/
https://www.mdpi.com/1420-3049/25/21/4930

 “Objectives: To investigate the action of cannabinoids on spasticity and pain in secondary progressive multiple sclerosis, by means of neurophysiological indexes.
“Objectives: To investigate the action of cannabinoids on spasticity and pain in secondary progressive multiple sclerosis, by means of neurophysiological indexes. “Multiple sclerosis (MS) is a highly symptomatic disease, with a wide range of disabilities affecting many bodily functions, even in younger persons with a short disease history.
“Multiple sclerosis (MS) is a highly symptomatic disease, with a wide range of disabilities affecting many bodily functions, even in younger persons with a short disease history.
 “To determine whether differences in disability status, spasticity severity, and spasticity duration at treatment start in patients with resistant multiple sclerosis (MS) spasticity might influence response to add-on tetrahydrocannabinol:
“To determine whether differences in disability status, spasticity severity, and spasticity duration at treatment start in patients with resistant multiple sclerosis (MS) spasticity might influence response to add-on tetrahydrocannabinol: “Treatment of spasticity poses a major challenge in amyotrophic lateral sclerosis (ALS) patient management.
“Treatment of spasticity poses a major challenge in amyotrophic lateral sclerosis (ALS) patient management.
