“A new face of endocannabinoids in pharmacotherapy. Part I: Protective role of endocannabinoids in hypertension and myocardial infarction.
Cannabinoids are compounds which were first isolated from the Cannabis sativa plant. For thousands of years they have been used for treatment of numerous diseases.
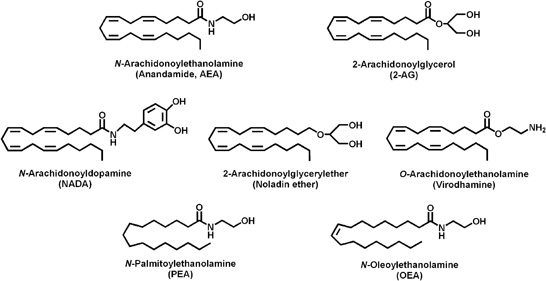
Currently, synthetic cannabinoids and endocannabinoids are also known. Cannabinoid receptors, endocannabinoids and the enzymes that catalyze their synthesis and degradation constitute the endocannabinoid system which plays an important role in functioning of the cardiovascular system.
The results obtained to date suggest the involvement of endocannabinoids in the pathology of many cardiovascular diseases, including myocardial infarction, hypertension and hypotension associated with hemorrhagic, endotoxic, and cardiogenic shock. Cardioprotective effect and dilation of coronary vessels induced by endocannabinoids deserve special attention.
It cannot be excluded now that in the future our better understanding of cannabinoid system will allow to develop new strategies for treatment of cardiovascular diseases.”
http://www.jpp.krakow.pl/journal/archive/04_14/pdf/171_04_14_article.pdf
“A new face of endocannabinoids in pharmacotherapy. Part II. Role of endocannabinoids in inflammation-derived cardiovaascular diseases.
Endocannabinoids play an important role in cardiovascular diseases caused by inflammatory disorders. Endocannabinoids are endogenous bioactive lipids that activate cannabinoid receptors and together with enzymes responsible for their synthesis and degradation constitute endocannabinoid system.
The results obtained to date suggest the involvement of endocannabinoids in the pathology of many cardiovascular diseases associated with inflammation, such as atherosclerosis, restenosis, chemotherapy-induced myocardial injury, diabetic and hepatic cirrhosis cardiomyopathy.
Our better understanding of cannabinoid system may result in the development of new strategies for the treatment of such disorders.”
http://www.jpp.krakow.pl/journal/archive/04_14/pdf/183_04_14_article.pdf

1942-7611/asset/olalertbanner.jpg?v=1&s=4b27d6a6bed6b58a9935efe70e4f95efc39146bd)

