
“The use of Cannabis sativa is currently recognized to ease certain types of chronic pain, reduce chemotherapy-induced nausea, and improve anxiety. Nevertheless, few studies highlighted the therapeutic potential of C. sativa extracts and related phytocannabinoids for a variety of widespread skin disorders including acne, atopic dermatitis, psoriasis, pruritus, and pain. This review summarized the current evidence on the effects of phytocannabinoids at the cutaneous level through the collection of in vitro, in vivo, and clinical studies published on PubMed, Scopus, Embase, and Web of Science until October 2020.
Phytocannabinoids have demonstrated potential anti-inflammatory, antioxidant, anti-aging, and anti-acne properties by various mechanisms involving either CB1/2-dependent and independent pathways.
Not only classical immune cells, but also several skin-specific actors, such as keratinocytes, fibroblasts, melanocytes, and sebocytes, may represent a target for phytocannabinoids. Cannabidiol, the most investigated compound, revealed photoprotective, antioxidant, and anti-inflammatory mechanisms at the cutaneous level, while the possible impact on cell differentiation, especially in the case of psoriasis, would require further investigation. Animal models and pilot clinical studies supported the application of cannabidiol in inflammatory-based skin diseases. Also, one of the most promising applications of non-psychotropic phytocannabinoids is the treatment of seborrheic disorders, especially acne. In conclusion, the incomplete knowledge of the role of the endocannabinoid system in skin disorders emerged as an important limit for pharmacological investigations. Moreover, the limited studies conducted on C. sativa extracts suggested a higher potency than single phytocannabinoids, thus stimulating new research on phytocannabinoid interaction.”
https://pubmed.ncbi.nlm.nih.gov/33851375/
https://www.thieme-connect.de/products/ejournals/abstract/10.1055/a-1420-5780

 “UV phototherapy used in chronic skin diseases causes redox imbalance and pro-inflammatory reactions, especially in the case of unchanged skin cells.
“UV phototherapy used in chronic skin diseases causes redox imbalance and pro-inflammatory reactions, especially in the case of unchanged skin cells. “Cannabidiol (CBD), a natural occurring phytocannabinoid, is used extensively in consumer products ranging from foods to shampoos, topical oils and lotions.
“Cannabidiol (CBD), a natural occurring phytocannabinoid, is used extensively in consumer products ranging from foods to shampoos, topical oils and lotions. “Psoriasis is associated with increased production of reactive oxygen species which leads to oxidative stress.
“Psoriasis is associated with increased production of reactive oxygen species which leads to oxidative stress.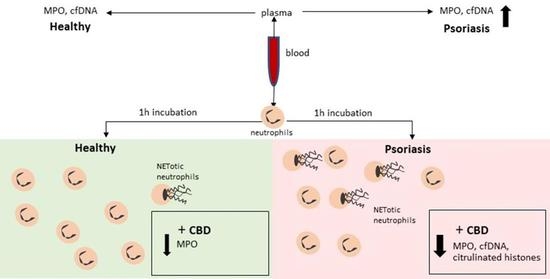
 “Psoriasis is a chronic inflammatory skin disease characterized by dysregulated keratinocyte differentiation, but oxidative stress also plays an important role in the pathogenesis of this disease.
“Psoriasis is a chronic inflammatory skin disease characterized by dysregulated keratinocyte differentiation, but oxidative stress also plays an important role in the pathogenesis of this disease. “The legalisation of
“The legalisation of  “Cannabinoids are increasingly-used substances in the treatment of chronic pain, some neuropsychiatric disorders and more recently, skin disorders with an inflammatory component.
“Cannabinoids are increasingly-used substances in the treatment of chronic pain, some neuropsychiatric disorders and more recently, skin disorders with an inflammatory component. “Medical marijuana is becoming widely available to patients in the U.S. and with recreational marijuana now legalized in many states, patient interest is on the rise.
“Medical marijuana is becoming widely available to patients in the U.S. and with recreational marijuana now legalized in many states, patient interest is on the rise. “Cannabis is increasingly being used world-wide to treat a variety of dermatological conditions. Medicinal cannabis is currently legalized in Canada, 31 states in America and 19 countries in Europe. The authors reviewed the literature on the pharmacology and use of
“Cannabis is increasingly being used world-wide to treat a variety of dermatological conditions. Medicinal cannabis is currently legalized in Canada, 31 states in America and 19 countries in Europe. The authors reviewed the literature on the pharmacology and use of