
“Women present increased susceptibility to anxiety- and stress-related disorders compared to men. A potentially promising pharmacological-based strategy to regulate abnormal aversive memories disrupts their reconsolidation stage after reactivation and destabilization.
Male rodent findings indicate that cannabidiol (CBD), a relatively safe and effective treatment for several mental health conditions, can impair the reconsolidation of aversive memories. However, whether and how CBD influences it in females is still unknown.
The present study addressed this question in contextually fear-conditioned female rats.
We report that systemically administered CBD impaired their reconsolidation, reducing freezing expression for over a week. This action was restricted to a time when the reconsolidation presumably lasted (< six hours post-retrieval) and depended on memory reactivation/destabilization. Moreover, the impairing effects of CBD on memory reconsolidation relied on the activation of cannabinoid type-1 but not type-2 receptors located in the CA1 subregion of the dorsal hippocampus.
CBD applied directly to this brain area was sufficient to reproduce the effects of systemic CBD treatment. Contextual fear memories attenuated by CBD did not show reinstatement, an extinction-related feature. By demonstrating that destabilized fear memories are sensitive to CBD and how it hinders mechanisms in the DH CA1 that may restabilize them in female rats, the present findings concur that reconsolidation blockers are viable and could be effective in disrupting abnormally persistent and distressing aversive memories such as those related to posttraumatic stress disorder.”
https://pubmed.ncbi.nlm.nih.gov/36049316/
https://www.sciencedirect.com/science/article/abs/pii/S0924977X22008367?via%3Dihub


 “The Cannabis sativa plant has been used medicinally and recreationally for thousands of years, but recently only relatively some of its constituents have been identified.
“The Cannabis sativa plant has been used medicinally and recreationally for thousands of years, but recently only relatively some of its constituents have been identified.  “Emotional dysregulation and anxiety are common in people at clinical high risk for psychosis (CHR) and are associated with altered neural responses to emotional stimuli in the striatum and medial temporal lobe.
“Emotional dysregulation and anxiety are common in people at clinical high risk for psychosis (CHR) and are associated with altered neural responses to emotional stimuli in the striatum and medial temporal lobe. “There is no argument with regard to the physical and psychological stress-related nature of neuropsychiatric disorders. Yet, the mechanisms that facilitate disease onset starting from molecular stress responses are elusive.
“There is no argument with regard to the physical and psychological stress-related nature of neuropsychiatric disorders. Yet, the mechanisms that facilitate disease onset starting from molecular stress responses are elusive.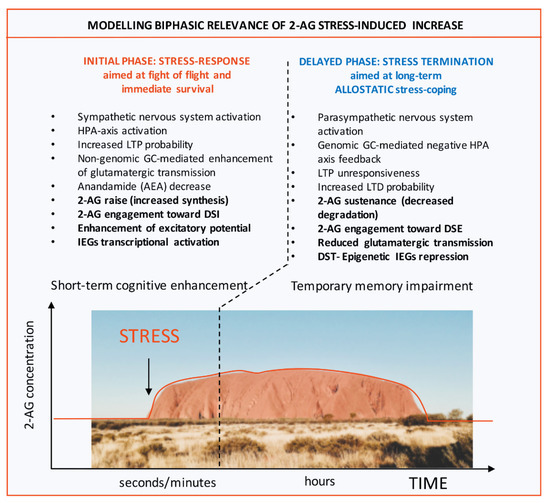
 “The endocannabinoid signaling system (ECSS) is altered by exposure to stress and mediates and modulates the effects of stress on the brain.
“The endocannabinoid signaling system (ECSS) is altered by exposure to stress and mediates and modulates the effects of stress on the brain. “Posttraumatic stress disorder (PTSD) may stem from the formation of aberrant and enduring aversive memories. Some PTSD patients have recreationally used Cannabis, probably aiming at relieving their symptomatology.
“Posttraumatic stress disorder (PTSD) may stem from the formation of aberrant and enduring aversive memories. Some PTSD patients have recreationally used Cannabis, probably aiming at relieving their symptomatology. “Posttraumatic stress disorder (PTSD) is an often chronic condition for which currently available medications have limited efficacy.
“Posttraumatic stress disorder (PTSD) is an often chronic condition for which currently available medications have limited efficacy. “The major phytocannabinoid cannabidiol (
“The major phytocannabinoid cannabidiol (