
Here, we explored the role of the cannabinoid system in muscle plasticity through the expression of muscle cannabinoid receptors (CBs) in young and old humans.
The CB1 expression was higher (+ 25%; p = 0.04) in muscle of old (≥ 65 years) vs. young adults (20-27 years), whereas CB2 was not differently expressed. Furthermore, resistance exercise tended to increase the CB1 (+ 11%; p = 0.055) and CB2 (+ 37%; p = 0.066) expression in muscle of older adults. Interestingly, increases in the expression of CB2 following resistance exercise positively correlated with changes in key mechanisms of muscle homeostasis, such as catabolism (FOXO3a) and regenerative capacity (Pax7, MyoD).
This study for the first time shows that CB1 is differentially expressed with aging and that changes in CB2 expression upon resistance exercise training correlate with changes in mediators that play a central role in muscle plasticity.
These data confirm earlier work in cells and mice showing that the cannabinoid system might orchestrate muscle growth, which is an incentive to further explore CB-based strategies that might counteract sarcopenia.”
“In conclusion, cell culture and murine experiments suggested that CBs can be a promising target to treat cachexia and sarcopenia through modulation of the metabolism and muscle regenerative capacity. These data imply that CB modulation might be a promising tool to combat muscle degeneration. ”

 “Background:
“Background:  “Cannabidiol is increasingly considered for treatment of a wide range of medical conditions.
“Cannabidiol is increasingly considered for treatment of a wide range of medical conditions.  “Background and purpose:
“Background and purpose:  “∆ 9 -Tetrahydrocannabinol (∆9 -THC), the active phytocannabinoid in cannabis, is virtually an adjunct to the endogenous endocannabinoid signaling system.
“∆ 9 -Tetrahydrocannabinol (∆9 -THC), the active phytocannabinoid in cannabis, is virtually an adjunct to the endogenous endocannabinoid signaling system. “There is no argument with regard to the physical and psychological stress-related nature of neuropsychiatric disorders. Yet, the mechanisms that facilitate disease onset starting from molecular stress responses are elusive.
“There is no argument with regard to the physical and psychological stress-related nature of neuropsychiatric disorders. Yet, the mechanisms that facilitate disease onset starting from molecular stress responses are elusive.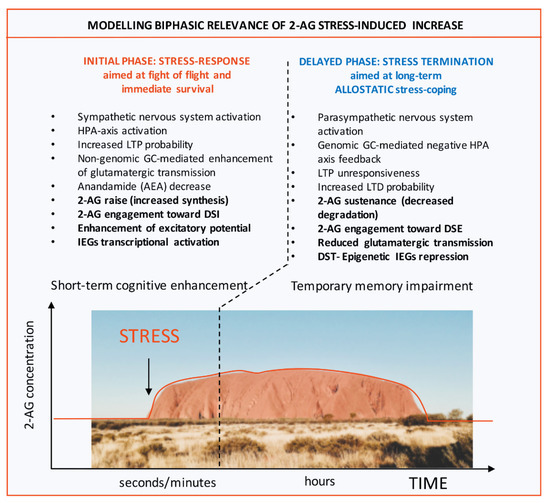
 “The endocannabinoid signaling system (ECSS) is altered by exposure to stress and mediates and modulates the effects of stress on the brain.
“The endocannabinoid signaling system (ECSS) is altered by exposure to stress and mediates and modulates the effects of stress on the brain. “Coronavirus disease 2019 (COVID-19) is spreading fast all around the world with more than fourteen millions of detected infected cases and more than 600.000 deaths by 20th July 2020. While scientist are working to find a vaccine, current epidemiological data shows that the most common comorbidities for patients with the worst prognosis, hypertension and diabetes, are often treated with angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs).
“Coronavirus disease 2019 (COVID-19) is spreading fast all around the world with more than fourteen millions of detected infected cases and more than 600.000 deaths by 20th July 2020. While scientist are working to find a vaccine, current epidemiological data shows that the most common comorbidities for patients with the worst prognosis, hypertension and diabetes, are often treated with angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs). “Although several lines of evidence support the hypothesis of a dysregulation of serotoninergic neurotransmission in the pathophysiology of obsessive-compulsive disorder (OCD), there is also evidence for an involvement of other pathways such as the GABAergic, glutamatergic, and dopaminergic systems.
“Although several lines of evidence support the hypothesis of a dysregulation of serotoninergic neurotransmission in the pathophysiology of obsessive-compulsive disorder (OCD), there is also evidence for an involvement of other pathways such as the GABAergic, glutamatergic, and dopaminergic systems.