 “Importance: Frontline health care professionals who work with patients with COVID-19 have an increased incidence of burnout symptoms. Cannabidiol (CBD) has anxiolytic and antidepressant properties and may be capable of reducing emotional exhaustion and burnout symptoms.
“Importance: Frontline health care professionals who work with patients with COVID-19 have an increased incidence of burnout symptoms. Cannabidiol (CBD) has anxiolytic and antidepressant properties and may be capable of reducing emotional exhaustion and burnout symptoms.
Objective: To investigate the safety and efficacy of CBD therapy for the reduction of emotional exhaustion and burnout symptoms among frontline health care professionals working with patients with COVID-19.
Interventions: Cannabidiol, 300 mg (150 mg twice per day), plus standard care or standard care alone for 28 days.
Main outcomes and measures: The primary outcome was emotional exhaustion and burnout symptoms, which were assessed for 28 days using the emotional exhaustion subscale of the Brazilian version of the Maslach Burnout Inventory-Human Services Survey for Medical Personnel.
Results: A total of 120 participants were randomized to receive either CBD, 300 mg, plus standard care (treatment arm; n = 61) or standard care alone (control arm; n = 59) for 28 days. Of those, 118 participants (59 participants in each arm; 79 women [66.9%]; mean age, 33.6 years [95% CI, 32.3-34.9 years]) received the intervention and were included in the efficacy analysis. In the treatment arm, scores on the emotional exhaustion subscale of the Maslach Burnout Inventory significantly decreased at day 14 (mean difference, 4.14 points; 95% CI, 1.47-6.80 points; partial eta squared [ηp2] = 0.08), day 21 (mean difference, 4.34 points; 95% CI, 0.94-7.73 points; ηp2 = 0.05), and day 28 (mean difference, 4.01 points; 95% CI, 0.43-7.59 points; ηp2 = 0.04). However, 5 participants, all of whom were in the treatment group, experienced serious adverse events: 4 cases of elevated liver enzymes (1 critical and 3 mild, with the mild elevations reported at the final 28-day assessment) and 1 case of severe pharmacodermia. In 2 of those cases (1 with critical elevation of liver enzymes and 1 with severe pharmacodermia), CBD therapy was discontinued, and the participants had a full recovery.
Conclusions and relevance: In this study, CBD therapy reduced symptoms of burnout and emotional exhaustion among health care professionals working with patients during the COVID-19 pandemic. However, it is necessary to balance the benefits of CBD therapy with potential undesired or adverse effects. Future double-blind placebo-controlled clinical trials are needed to confirm the present findings.”
https://pubmed.ncbi.nlm.nih.gov/34387679/
“Daily administration of CBD, 300 mg, combined with standard care reduced the symptoms and diagnoses of anxiety, depression, and emotional exhaustion among frontline health care professionals working with patients with COVID-19. Cannabidiol may act as an effective agent for the reduction of burnout symptoms among a population with important mental health needs worldwide.”
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2782994


 “Colic is a common digestive disorder in horses and one of the most urgent problems in equine medicine. A growing body of literature has indicated that the activation of cannabinoid receptors could exert beneficial effects on gastrointestinal inflammation and visceral hypersensitivity.
“Colic is a common digestive disorder in horses and one of the most urgent problems in equine medicine. A growing body of literature has indicated that the activation of cannabinoid receptors could exert beneficial effects on gastrointestinal inflammation and visceral hypersensitivity.  “Background:
“Background:  “Cannabidiol is increasingly considered for treatment of a wide range of medical conditions.
“Cannabidiol is increasingly considered for treatment of a wide range of medical conditions.  “Background and purpose:
“Background and purpose: 
 “Despite the high incidence of traumatic brain injury (TBI), there is no universal treatment to safely treat patients. Blunt brain injuries destroy primary neural tissue that results in impaired perfusion, excessive release of glutamate, inflammation, excitotoxicity, and progressive secondary neuronal cell death.
“Despite the high incidence of traumatic brain injury (TBI), there is no universal treatment to safely treat patients. Blunt brain injuries destroy primary neural tissue that results in impaired perfusion, excessive release of glutamate, inflammation, excitotoxicity, and progressive secondary neuronal cell death.  “Importance:
“Importance:  “Studies investigating the psychosomatic effects of social isolation in animals have shown that one of the physiologic system that gets disrupted by this environment-affective change is the Endocannabinoid System. As the levels of endocannabinoids change in limbic areas and prefrontal cortex during stressful times, so is the subject more prone to fearful and negative thoughts and aggressive behavior. The interplay of social isolation on the hypothalamic-pituitary-adrenal axis and cannabinoid tone triggers a vicious cycle which further impairs the natural body’s homeostatic neuroendocrine levels and provokes a series of risk factors for developing health complications. In this paper, we explore the psychosomatic impact of prolonged quarantine in healthy individuals, and propose management and coping strategies that may improve endocannabinoid tone, such as integration of probiotics, cannabidiol, meditation, and physical exercise interventions with the aim of supporting interpersonal, individual, and professional adherence with COVID-19 emergency public measures whilst minimizing their psycho-physical impact.”
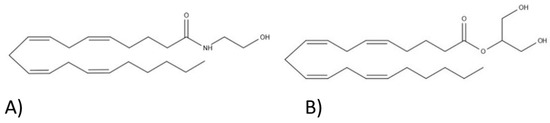
“Studies investigating the psychosomatic effects of social isolation in animals have shown that one of the physiologic system that gets disrupted by this environment-affective change is the Endocannabinoid System. As the levels of endocannabinoids change in limbic areas and prefrontal cortex during stressful times, so is the subject more prone to fearful and negative thoughts and aggressive behavior. The interplay of social isolation on the hypothalamic-pituitary-adrenal axis and cannabinoid tone triggers a vicious cycle which further impairs the natural body’s homeostatic neuroendocrine levels and provokes a series of risk factors for developing health complications. In this paper, we explore the psychosomatic impact of prolonged quarantine in healthy individuals, and propose management and coping strategies that may improve endocannabinoid tone, such as integration of probiotics, cannabidiol, meditation, and physical exercise interventions with the aim of supporting interpersonal, individual, and professional adherence with COVID-19 emergency public measures whilst minimizing their psycho-physical impact.” “Cannabis sativa
“Cannabis sativa