“Background: Cannabidiol (CBD), one major nonintoxicating phytocannabinoid from Cannabis sativa demonstrated anti-inflammatory effects in animal models of several inflammatory conditions, including arthritis. However, it is still unknown which cell types mediate these anti-inflammatory effects of CBD, and, since CBD binds to a plethora of receptors and enzymes, it is complicated to pinpoint its mechanism of action. In this study, we elucidate the effects of CBD on B cells and peripheral blood mononuclear cells (PBMCs) in respect to survival, calcium mobilization, drug uptake, and cytokine (IL-6, IL-10, and TNF) and immunoglobulin production.
Methods: Modulation of intracellular calcium and drug uptake in B cells was determined by using the fluorescent dyes Cal-520 and PoPo3, respectively. Cytokine and immunoglobulin production was evaluated by enzyme-linked immunosorbent assay. PBMC composition and B cell survival after CBD treatment was assessed by flow cytometry.
Results: B cells express two major target receptors for CBD, TRPV2 (transient receptor potential vanilloid 2) and TRPA1 (transient receptor potential ankyrin 1), which are not regulated by B cell activation. CBD increased intracellular calcium levels in mouse and human B cells, which was accompanied by enhanced uptake of PoPo3. These effects were not dependent on transient receptor potential channel activation. CBD increased the number of early apoptotic B cells at the expense of viable cells and diminished interleukin (IL)-10 and tumor necrosis factor (TNF) production when activated T cell independently. In PBMCs, CBD increased IL-10 production when B cells were activated T cell dependent, while decreasing TNF levels when activated T cell independently. In PBMC/rheumatoid synovial fibroblast cocultures, CBD reduced IL-10 production when B cells were activated T cell independently. Immunoglobulin M production was augmented by CBD when B cells were activated with CpG.
Conclusion: CBD is able to provide pro- and anti-inflammatory effects in isolated B cells and PBMCs. This is dependent on the activating stimulus (T cell dependent or independent) and concentration of CBD. Therefore, CBD might be used to dampen B cell activity in autoimmune conditions such as rheumatoid arthritis, in which B cells are activated by specific autoantigens.”



 “The generation of functional regulatory T cells (Tregs) is essential to keep tissue homeostasis and restore healthy immune responses in many biological and inflammatory contexts.
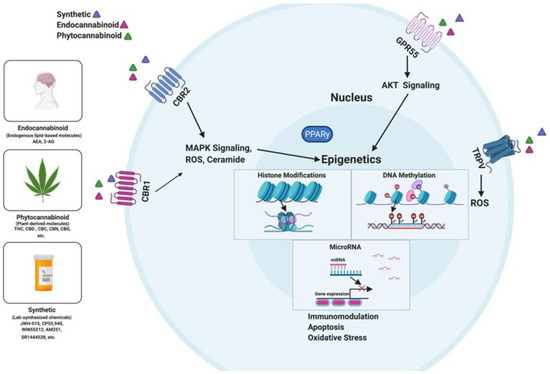
“The generation of functional regulatory T cells (Tregs) is essential to keep tissue homeostasis and restore healthy immune responses in many biological and inflammatory contexts.  “The Endocannabinoid System (ECS) is primarily responsible for maintaining homeostasis, a balance in internal environment (temperature, mood, and immune system) and energy input and output in living, biological systems.
“The Endocannabinoid System (ECS) is primarily responsible for maintaining homeostasis, a balance in internal environment (temperature, mood, and immune system) and energy input and output in living, biological systems.  “Background and purpose:
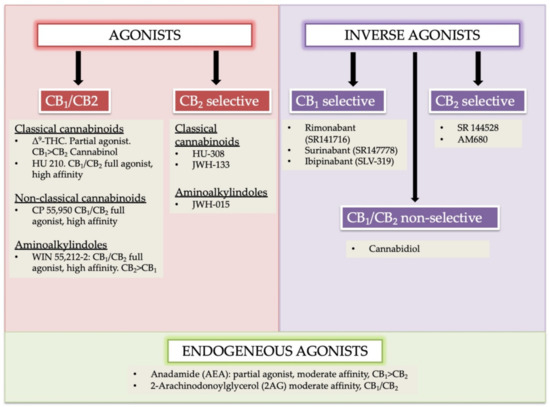
“Background and purpose:  “In humans, various sites like cannabinoid receptors (CBR) having a binding affinity with cannabinoids are distributed on the surface of different cell types, where endocannabinoids (ECs) and derivatives of fatty acid can bind. The binding of these substance(s) triggers the activation of specific receptors required for various physiological functions, including pain sensation, memory, and appetite.
“In humans, various sites like cannabinoid receptors (CBR) having a binding affinity with cannabinoids are distributed on the surface of different cell types, where endocannabinoids (ECs) and derivatives of fatty acid can bind. The binding of these substance(s) triggers the activation of specific receptors required for various physiological functions, including pain sensation, memory, and appetite.