 “Ehlers-Danlos Syndromes (EDS) and related Hypermobility Spectrum Disorders (HSD) are debilitating connective tissue disorders that feature a prominent pain component for which there are limited therapeutic options for pain management.
“Ehlers-Danlos Syndromes (EDS) and related Hypermobility Spectrum Disorders (HSD) are debilitating connective tissue disorders that feature a prominent pain component for which there are limited therapeutic options for pain management.
Consequently, many patients try various non-prescribed treatments, including complementary and alternative therapies that have not been well studied in the EDS/HSD patient population. We surveyed over 500 individuals through the EDS Society who reported having been diagnosed with EDS or HSD to ascertain what complementary and alternative therapies were used and their reported effectiveness in alleviating pain and improving quality of life.
Specifically, we focused on the use of traditional Chinese therapies, herbal medications, and marijuana.
The most commonly reported therapies, used by 70-92% of participants, were non-steroidal anti-inflammatory drugs, acetaminophen, opioids, and physical therapy.
Therapies rated by participants as most efficacious were opioids, physical therapy, and marijuana with 10-24% of those using these therapies rating them as extremely helpful.
Patient-initiated complementary therapy use in EDS/HSD patients is widespread at 56%. Complementary therapies were largely utilized by EDS/HSD patients with higher reported pain levels. Providers caring for EDS/HSD patients should be aware of these data showing broad usage of predominantly non-prescribed therapies and be prepared to consider such usage in working collaboratively with these patients to develop comprehensive treatment plans to manage their chronic pain complications.”

 “We present the case of an 18-year-old woman who suffered from complications of Ehlers-Danlos syndrome (EDS). Her pain was poorly controlled despite being on a myriad of analgesic medications at the time.
“We present the case of an 18-year-old woman who suffered from complications of Ehlers-Danlos syndrome (EDS). Her pain was poorly controlled despite being on a myriad of analgesic medications at the time. “Central pain after stroke due to brainstem infarction is very rare. Treatment is difficult and specific guidelines are lacking. This is the report of a 61-year-old female patient who, after a posterolateral left medulla oblongata insult with incomplete Wallenberg syndrome, subsequently developed a burning and tingling pain in the contralateral leg and a burning and shooting pain in the ipsilateral face in trigeminal branches 1 and 2. More than 3 years of therapy with amitriptyline, gabapentin, pregabalin and various grade II and III opioids was ineffective or showed intolerable side effects. The administration of tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio improved the pain situation and quality of life quickly and permanently. The encouraging results in the present case may suggest that treatment with medical cannabis should be considered in similar cases when standard therapies are insufficient.”
“Central pain after stroke due to brainstem infarction is very rare. Treatment is difficult and specific guidelines are lacking. This is the report of a 61-year-old female patient who, after a posterolateral left medulla oblongata insult with incomplete Wallenberg syndrome, subsequently developed a burning and tingling pain in the contralateral leg and a burning and shooting pain in the ipsilateral face in trigeminal branches 1 and 2. More than 3 years of therapy with amitriptyline, gabapentin, pregabalin and various grade II and III opioids was ineffective or showed intolerable side effects. The administration of tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio improved the pain situation and quality of life quickly and permanently. The encouraging results in the present case may suggest that treatment with medical cannabis should be considered in similar cases when standard therapies are insufficient.” “
“ “
“ “The therapeutic potential of
“The therapeutic potential of 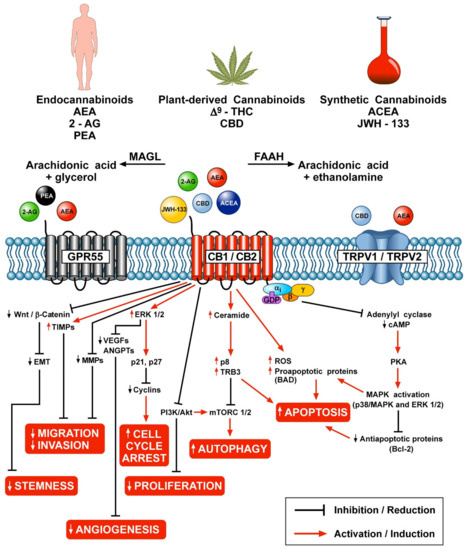
 “Cannabinoids, including delta-8- and delta-9-tetrahydrocannabinol (THC) have a palliative care impact and may therefore be beneficial against cancer.
“Cannabinoids, including delta-8- and delta-9-tetrahydrocannabinol (THC) have a palliative care impact and may therefore be beneficial against cancer.  “Background:
“Background: