 “Stem cell therapy promotes tissue regeneration and wound healing. Efforts have been made to prime stem cells to enhance their regenerative abilities.
“Stem cell therapy promotes tissue regeneration and wound healing. Efforts have been made to prime stem cells to enhance their regenerative abilities.
Certain marijuana components, namely the non-psychoactive cannabidiol (CBD) and psychoactive tetrahydrocannabinol (THC), are defined as immunomodulators.9 We test whether two sources of stem cells, primed with CBD or THC, would demonstrate improved regenerative abilities.
Human adipose-derived stem cells (ASCs) and bone marrow-derived stem cells (BMDSCs), not obtained from the same individual, were treated with low (300 nM) or high (3 μM) concentration CBD. Porcine ASCs and BMDSCs were isolated from a single pig, and treated with either low or high concentrations of CBD or THC. Transwell migration and MTT proliferation assays were performed on the human ASCs and BMDSCs. Also, transwell migration assay was performed on the porcine ASCs and BMDSCs. Finally, a wound healing scratch assay in porcine primary fibroblasts (PFs) was performed, co-cultured with the cannabinoid-treated ASCs.
CBD priming at low concentration induces migration by 180% (P < .01) in porcine ASCs, and by only 93% (P < .02) in porcine BMDSCs. In porcine stem cells, THC priming at low concentration induces migration by 91.6% (P < .01) in ASCs but by only 44.3% (P < .03) in BMDSCs. Compared to PFs co-cultured with untreated ASCs, PFs co-cultured with low CBD-primed ASCs had 75% faster wound closure at 18 hours (P < .01).
CBD and THC priming of ASCs and BMDSCs, particularly at lower doses, enhances a number of regenerative parameters, suggesting that these major marijuana components may improve stem cell-based therapies.
SIGNIFICANCE OF THE STUDY: Our study demonstrates that cannabinoids can enhance the regenerative capacity of two major sources of stem cells, adipose- and bone marrow-derived, from human and porcine donors. Stem cell isolation and expansion is invasive, costly and time consuming. Stem cells with improved regenerative properties may be effective in the treatment of acute or chronic wounds. This is the first study to compare the priming potential of two sources of stem cells from the same animal, with the same genetic and epigenetic profile, as well as the first to prime with THC.”

 “A significant number of cannabinoids are known to have analgesic and anti-inflammatory properties in various diseases. Due to their presynaptic/terminal location, cannabinoid receptors can inhibit synaptic transmission and have the potential to regulate neurogenic inflammation. Neurogenic inflammation occurs when a noxious signal is detected in the periphery initiating an antidromic axon reflex in the same sensory neurone leading to depolarization of the afferent terminal. Neuropeptides are subsequently released and contribute to vasodilation, plasma extravasation and modulation of immune cells. Endocannabinoids, synthetic cannabinoids and phytocannabinoids can reduce neuroinflammation by inhibiting afferent firing and inflammatory neuropeptide release. Thus, in addition to a direct effect on vascular smooth muscle and inflammatory cells, cannabinoids can reduce inflammation by silencing small diameter neurones. This review examines the neuropharmacological processes involved in regulating antidromic depolarization of afferent nerve terminals by cannabinoids and the control of neurogenic inflammation in different diseases.”
“A significant number of cannabinoids are known to have analgesic and anti-inflammatory properties in various diseases. Due to their presynaptic/terminal location, cannabinoid receptors can inhibit synaptic transmission and have the potential to regulate neurogenic inflammation. Neurogenic inflammation occurs when a noxious signal is detected in the periphery initiating an antidromic axon reflex in the same sensory neurone leading to depolarization of the afferent terminal. Neuropeptides are subsequently released and contribute to vasodilation, plasma extravasation and modulation of immune cells. Endocannabinoids, synthetic cannabinoids and phytocannabinoids can reduce neuroinflammation by inhibiting afferent firing and inflammatory neuropeptide release. Thus, in addition to a direct effect on vascular smooth muscle and inflammatory cells, cannabinoids can reduce inflammation by silencing small diameter neurones. This review examines the neuropharmacological processes involved in regulating antidromic depolarization of afferent nerve terminals by cannabinoids and the control of neurogenic inflammation in different diseases.” “Effective treatment choices to the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) are limited because of the absence of effective target-based therapeutics. The main object of the current research was to estimate the antiviral activity of cannabinoids (CBDs) against the human coronavirus SARS-CoV-2.
“Effective treatment choices to the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) are limited because of the absence of effective target-based therapeutics. The main object of the current research was to estimate the antiviral activity of cannabinoids (CBDs) against the human coronavirus SARS-CoV-2.
 “Chronic adolescent exposure to Δ-9-Tetrahydrocannabinol (THC) is linked to elevated neuropsychiatric risk and induces neuronal, molecular and behavioural abnormalities resembling neuropsychiatric endophenotypes. Previous evidence has revealed that the mesocorticolimbic circuitry, including the prefrontal cortex (PFC) and mesolimbic dopamine (DA) pathway are particularly susceptible to THC-induced pathological alterations, including dysregulation of DAergic activity states, loss of PFC GABAergic inhibitory control and affective and cognitive abnormalities. There are currently limited pharmacological intervention strategies capable of preventing THC-induced neuropathological adaptations.
“Chronic adolescent exposure to Δ-9-Tetrahydrocannabinol (THC) is linked to elevated neuropsychiatric risk and induces neuronal, molecular and behavioural abnormalities resembling neuropsychiatric endophenotypes. Previous evidence has revealed that the mesocorticolimbic circuitry, including the prefrontal cortex (PFC) and mesolimbic dopamine (DA) pathway are particularly susceptible to THC-induced pathological alterations, including dysregulation of DAergic activity states, loss of PFC GABAergic inhibitory control and affective and cognitive abnormalities. There are currently limited pharmacological intervention strategies capable of preventing THC-induced neuropathological adaptations. “Cannabis sativa is a well-known plant which has been of benefit since ancient times in several medicinal systems, including Chinese, Indian, Greek and Egyptian ones.
“Cannabis sativa is a well-known plant which has been of benefit since ancient times in several medicinal systems, including Chinese, Indian, Greek and Egyptian ones. “In the last decade the use of medical cannabis (MC) for palliative cancer treatment has risen. However, the choice between products is arbitrary and most patients are using Tetrahydrocannabinol (THC)-dominant cannabis products.
“In the last decade the use of medical cannabis (MC) for palliative cancer treatment has risen. However, the choice between products is arbitrary and most patients are using Tetrahydrocannabinol (THC)-dominant cannabis products. “UV radiation is a well-established environmental risk factor known to cause oxidative stress and disrupt the metabolism of keratinocyte phospholipids. Cannabidiol (CBD) is a phytocannabinoid with anti-inflammatory and antioxidant effects.
“UV radiation is a well-established environmental risk factor known to cause oxidative stress and disrupt the metabolism of keratinocyte phospholipids. Cannabidiol (CBD) is a phytocannabinoid with anti-inflammatory and antioxidant effects.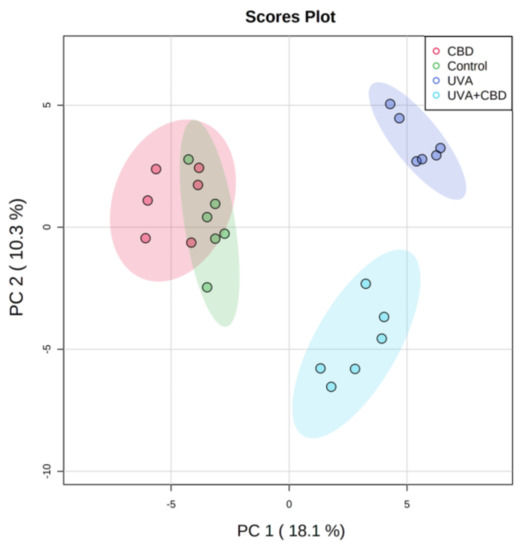
 “Leukocytes are part of the tumor microenvironment (TME) and are critical determinants of tumor progression. Because of the immunoregulatory properties of cannabinoids, the endocannabinoid system (ECS) may have an important role in shaping the TME.
“Leukocytes are part of the tumor microenvironment (TME) and are critical determinants of tumor progression. Because of the immunoregulatory properties of cannabinoids, the endocannabinoid system (ECS) may have an important role in shaping the TME.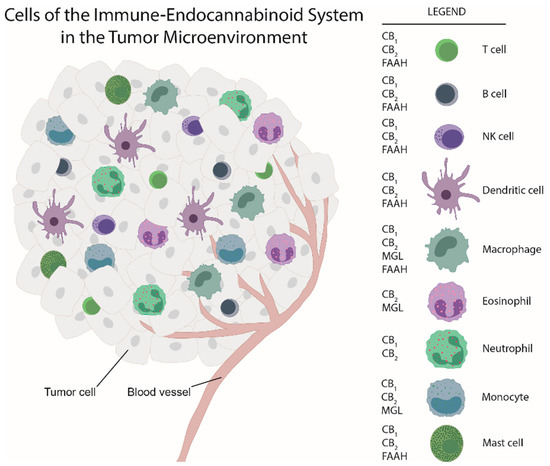
 “There is not a single pharmacological agent with demonstrated therapeutic efficacy for traumatic brain injury (TBI). With recent legalization efforts and the growing popularity of medical cannabis, patients with TBI will inevitably consider medical cannabis as a treatment option.
“There is not a single pharmacological agent with demonstrated therapeutic efficacy for traumatic brain injury (TBI). With recent legalization efforts and the growing popularity of medical cannabis, patients with TBI will inevitably consider medical cannabis as a treatment option.