 “Chronic hepatitis B virus (HBV) infection may evolve into cirrhosis and hepatocellular carcinoma, and this progression may be accelerated by specific risk factors, including overweight and obesity. Although evidence for a protective effect of cannabis use on elevated body weight has been found for other populations, no data are available for HBV-infected patients.
“Chronic hepatitis B virus (HBV) infection may evolve into cirrhosis and hepatocellular carcinoma, and this progression may be accelerated by specific risk factors, including overweight and obesity. Although evidence for a protective effect of cannabis use on elevated body weight has been found for other populations, no data are available for HBV-infected patients.
Aims: We aimed to identify risk factors (including cannabis use) for overweight and obesity in patients with HBV chronic infection.
Methods: Using baseline data from the French ANRS CO22 Hepather cohort, we performed two separate analyses, one using “central obesity” (based on waist circumference) and the other “overweight” and “obesity” (based on body mass index) as outcomes. Logistic and multinomial regressions were used to model central obesity and overweight/obesity, respectively.
Results: Among the 3706 patients in the study population, 50.8% had central obesity, 34.7% overweight, and 14.4% obesity. After multivariable adjustment, current cannabis use was associated with a 59% lower risk of central obesity compared with no lifetime use (adjusted odds ratio [95% CI]: 0.41 [0.24 to 0.70]). It was also associated with a 54% and 84% lower risk of overweight (adjusted relative risk ratio [95% CI]: 0.46 [0.27 to 0.76]) and obesity (0.16 [0.04 to 0.67]), respectively.
Conclusions: Cannabis use was associated with lower risks of overweight and obesity in patients with HBV chronic infection. Future studies should test whether these potential benefits of cannabis and cannabinoid use translate into reduced liver disease progression in this high-risk population.”

 “Interest in CBG (cannabigerol) has been growing in the past few years, due to its anti-inflammatory properties and other therapeutic benefits.
“Interest in CBG (cannabigerol) has been growing in the past few years, due to its anti-inflammatory properties and other therapeutic benefits. 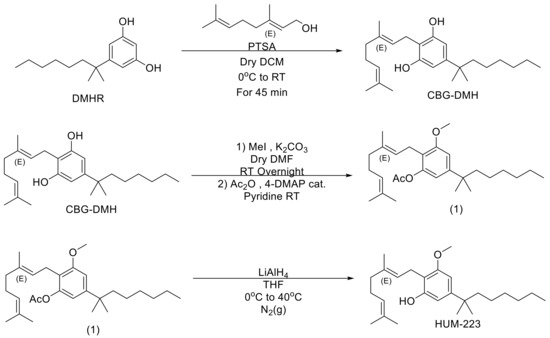
 “Beta-Caryophyllene (BCP), a naturally occurring sesquiterpene abundantly found in cloves, hops, and cannabis, is the active candidate of a relatively new group of vascular-inhibiting compounds that aim to block existing tumor blood vessels.
“Beta-Caryophyllene (BCP), a naturally occurring sesquiterpene abundantly found in cloves, hops, and cannabis, is the active candidate of a relatively new group of vascular-inhibiting compounds that aim to block existing tumor blood vessels.  “Acute respiratory distress syndrome (ARDS) is a life-threatening clinical syndrome whose potential to become one of the most grievous challenges of the healthcare system evidenced by the COVID-19 pandemic. Considering the lack of target-specific treatment for ARDS, it is absolutely exigent to have an effective therapeutic modality to reduce hospitalization and mortality rate as well as to improve quality of life and outcomes for ARDS patients. ARDS is a systemic inflammatory disease starting with the pulmonary system and involves all other organs in a morbid bidirectional fashion. Mounting evidence including our findings supporting the notion that cannabinoids have potential to be targeted as regulatory therapeutic modalities in the treatment of inflammatory diseases. Therefore, it is plausible to test their capabilities as alternative therapies in the treatment of ARDS. In this study, we investigated the potential protective effects of cannabichromene (CBC) in an experimental model of ARDS.
“Acute respiratory distress syndrome (ARDS) is a life-threatening clinical syndrome whose potential to become one of the most grievous challenges of the healthcare system evidenced by the COVID-19 pandemic. Considering the lack of target-specific treatment for ARDS, it is absolutely exigent to have an effective therapeutic modality to reduce hospitalization and mortality rate as well as to improve quality of life and outcomes for ARDS patients. ARDS is a systemic inflammatory disease starting with the pulmonary system and involves all other organs in a morbid bidirectional fashion. Mounting evidence including our findings supporting the notion that cannabinoids have potential to be targeted as regulatory therapeutic modalities in the treatment of inflammatory diseases. Therefore, it is plausible to test their capabilities as alternative therapies in the treatment of ARDS. In this study, we investigated the potential protective effects of cannabichromene (CBC) in an experimental model of ARDS. “The global incidence of respiratory diseases and complications is increasing. Therefore, new methods of treatment, as well as prevention, need to be investigated.
“The global incidence of respiratory diseases and complications is increasing. Therefore, new methods of treatment, as well as prevention, need to be investigated.  “THC, CBD, and CBN were reported as promising candidates against SARS-CoV2 infection, but the mechanism of action of these three cannabinoids is not understood.
“THC, CBD, and CBN were reported as promising candidates against SARS-CoV2 infection, but the mechanism of action of these three cannabinoids is not understood.  “Given the abundancy of angiotensin converting enzyme 2 (ACE-2) receptors density, beyond the lung, the intestine is considered as an alternative site of infection and replication for severe acute respiratory syndrome by coronavirus type 2 (SARS-CoV-2).
“Given the abundancy of angiotensin converting enzyme 2 (ACE-2) receptors density, beyond the lung, the intestine is considered as an alternative site of infection and replication for severe acute respiratory syndrome by coronavirus type 2 (SARS-CoV-2).  “This study consists of a brief psychological intervention, which uses Self-Regulation Therapy (SRT, procedure based on suggestion and classical conditioning), to improve coping with stress and emotionality by reproducing the positive effects of illegal drugs: cannabis, cocaine, ecstasy.
“This study consists of a brief psychological intervention, which uses Self-Regulation Therapy (SRT, procedure based on suggestion and classical conditioning), to improve coping with stress and emotionality by reproducing the positive effects of illegal drugs: cannabis, cocaine, ecstasy.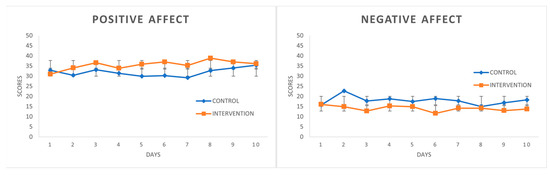
 “Conventional lung cancer treatments include surgery, chemotherapy and radiotherapy; however, these treatments are often poorly tolerated by patients. Cannabinoids have been studied for use as a primary cancer treatment. Cannabinoids, which are chemically similar to our own body’s endocannabinoids, can interact with signalling pathways to control the fate of cells, including cancer cells. We present a patient who declined conventional lung cancer treatment. Without the knowledge of her clinicians, she chose to self-administer ‘cannabidiol (CBD) oil’ orally 2-3 times daily. Serial imaging shows that her cancer reduced in size progressively from 41 mm to 10 mm over a period of 2.5 years. Previous studies have failed to agree on the usefulness of cannabinoids as a cancer treatment. This case appears to demonstrate a possible benefit of ‘CBD oil’ intake that may have resulted in the observed tumour regression. The use of cannabinoids as a potential cancer treatment justifies further research.”
“Conventional lung cancer treatments include surgery, chemotherapy and radiotherapy; however, these treatments are often poorly tolerated by patients. Cannabinoids have been studied for use as a primary cancer treatment. Cannabinoids, which are chemically similar to our own body’s endocannabinoids, can interact with signalling pathways to control the fate of cells, including cancer cells. We present a patient who declined conventional lung cancer treatment. Without the knowledge of her clinicians, she chose to self-administer ‘cannabidiol (CBD) oil’ orally 2-3 times daily. Serial imaging shows that her cancer reduced in size progressively from 41 mm to 10 mm over a period of 2.5 years. Previous studies have failed to agree on the usefulness of cannabinoids as a cancer treatment. This case appears to demonstrate a possible benefit of ‘CBD oil’ intake that may have resulted in the observed tumour regression. The use of cannabinoids as a potential cancer treatment justifies further research.” “Aims: Characterizing cannabinoid receptors (CBRs) expressed in Ewing sarcoma (EWS) cell lines as potential targets for anti-cancer drug development.
“Aims: Characterizing cannabinoid receptors (CBRs) expressed in Ewing sarcoma (EWS) cell lines as potential targets for anti-cancer drug development.