Abstract
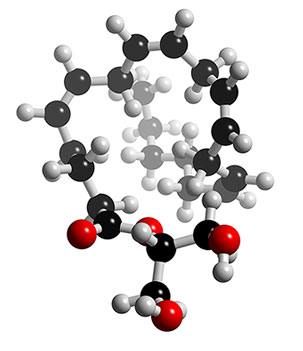
“A long-standing goal in cannabinoid research has been the discovery of potent synthetic analogs of the natural substances that might be developed as clinically useful drugs. This requires, among other things, that they be free of the psychotropic effects that characterize the recreational use of Cannabis. An important driving force for this goal is the long history of the use of Cannabis as a medicinal agent especially in the treatment of pain and inflammation. While few compounds appear to have these properties, ajulemic acid (AJA), also known as CT-3 and IP-751, is a potential candidate that could achieve this goal. Its chemical structure was derived from that of the major metabolite of Delta9-THC, the principal psychotropic constituent of Cannabis. In preclinical studies it displayed many of the properties of non-steroidal anti-inflammatory drugs (NSAIDs); however, it seems to be free of undesirable side effects. The initial short-term trials in healthy human subjects, as well as in patients with chronic neuropathic pain, demonstrated a complete absence of psychotropic actions. Moreover, it proved to be more effective than placebo in reducing this type of pain as measured by the visual analog scale. Unlike the narcotic analgesics, signs of dependency were not observed after withdrawal of the drug at the end of the one-week treatment period. Data on its mechanism of action are not yet complete; however, the activation of PPAR-gamma, and regulation of eicosanoid and cytokine production, appear to be important for its potential therapeutic effects.”

 mg/day for 6 weeks was found to be non-toxic, relative to placebo, in clinical trials; and because CBD reduced motility during inflammation and not in physiological conditions, CBD might be considered as a good candidate to be clinically evaluated for the treatment of hypermotility associated with inflammatory bowel disease.”
mg/day for 6 weeks was found to be non-toxic, relative to placebo, in clinical trials; and because CBD reduced motility during inflammation and not in physiological conditions, CBD might be considered as a good candidate to be clinically evaluated for the treatment of hypermotility associated with inflammatory bowel disease.”