 “To assess any clinical improvement attributable to the addition of medical cannabis treatment (MCT) to the stable (>3 months) standard analgesic treatment of fibromyalgia (FM) patients, the retention rate and any changes in the concomitant analgesic treatment over a period of six months.
“To assess any clinical improvement attributable to the addition of medical cannabis treatment (MCT) to the stable (>3 months) standard analgesic treatment of fibromyalgia (FM) patients, the retention rate and any changes in the concomitant analgesic treatment over a period of six months.
METHODS:
The study involved 102 consecutive FM patients with VAS scores ≥4 despite standard analgesic treatment. Patients were prescribed two oil-diluted cannabis extracts: Bedrocan (22% THC, <1% CBD), and Bediol (6.3% THC, 8% CBD). FM severity was periodically assessed using Fibromyalgia Impact Questionnaire (FIQR), Fibromyalgia Assessment Scale (FAS), FACIT-Fatigue score, Pittsburgh Sleep Quality Index (PSQI), and Zung Depression and Anxiety Scales. During the study, patients were allowed to reduce or stop their concomitant analgesic therapy.
RESULTS:
The 6-month retention rate was 64%. A significant improvement in the PSQI and FIQR was observed in respectively 44% and 33% of patients. 50% showed a moderate improvement in the anxiety and depression scales. Multiple regression analysis showed a correlation between the body mass index (BMI) and FIQR improvement (p=0.017). Concomitant analgesic treatment was reduced or suspended in 47% of the patients. One-third experienced mild adverse events, which did not cause any significant treatment modifications.
CONCLUSIONS:
This observational study shows that adjunctive MCT offers a possible clinical advantage in FM patients, especially in those with sleep dysfunctions. The clinical improvement inversely correlated with BMI. The retention rate and changes in concomitant analgesic therapy reflect MCT efficacy of the improved quality of life of patients. Further studies are needed to confirm these data, identify MCT-responsive sub-groups of FM patients, and establish the most appropriate posology and duration of the therapy.”

 “While medical and recreational cannabis use is becoming more frequent among older adults, the neurocognitive consequences of cannabis use in this age group are unclear. The aim of this literature review was to synthesize and evaluate the current knowledge on the association of cannabis use during older-adulthood with cognitive function and brain aging.
“While medical and recreational cannabis use is becoming more frequent among older adults, the neurocognitive consequences of cannabis use in this age group are unclear. The aim of this literature review was to synthesize and evaluate the current knowledge on the association of cannabis use during older-adulthood with cognitive function and brain aging.
 “Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
“Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).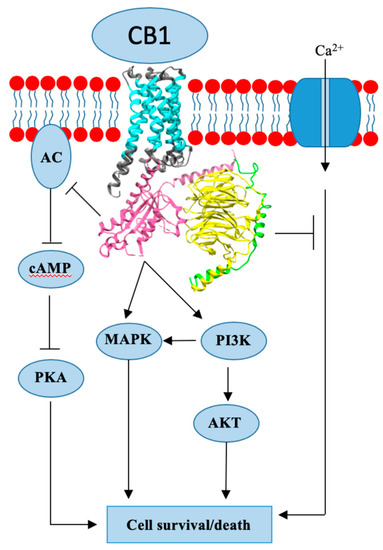
 “The 20% prevalence of chronic pain in the general population is a major health concern given the often profound associated impairment of daily activities, employment status, and health-related quality of life in sufferers. Resource utilization associated with chronic pain represents an enormous burden for healthcare systems. Although analgesia based on the World Health Organization’s pain ladder continues to be the mainstay of chronic pain management, aside from chronic cancer pain or end-of-life care, prolonged use of non-steroidal anti-inflammatory drugs or opioids to manage chronic pain is rarely sustainable.
“The 20% prevalence of chronic pain in the general population is a major health concern given the often profound associated impairment of daily activities, employment status, and health-related quality of life in sufferers. Resource utilization associated with chronic pain represents an enormous burden for healthcare systems. Although analgesia based on the World Health Organization’s pain ladder continues to be the mainstay of chronic pain management, aside from chronic cancer pain or end-of-life care, prolonged use of non-steroidal anti-inflammatory drugs or opioids to manage chronic pain is rarely sustainable. “Medicinal
“Medicinal  “A growing body of literature indicates that activation of
“A growing body of literature indicates that activation of  “Inflammatory Bowel Disease (IBD) is idiopathic, chronic and affects the gastrointestinal tract. It results from the association of genetic, environmental and immune deregulation, which culminates in the development and progression of the inflammatory process. In an attempt to reverse colonic inflammation, endogenous systems involved in intestinal physiology are studied and the cholinergic system is fundamental for this process. In addition, this system has anti-inflammatory action in experimental models of IBD. Another important endogenous system in regulating the exacerbated inflammatory response in the gut is mediated by endocannabinoids, which play an important role in restoring bowel functionality after the onset of the inflammatory process. There are several reports in the literature showing the interconnection between the cannabinoid and cholinergic systems in different tissues. Considering that the activation of the cholinergic system stimulates the production of cannabinoid agonists in the intestine, our hypothesis is that the interaction between the muscarinic system and the cannabinoid in the control of intestinal inflammation is mediated by endogenous cannabinoids, since they are stimulated by the activation of muscarinic receptors.”
“Inflammatory Bowel Disease (IBD) is idiopathic, chronic and affects the gastrointestinal tract. It results from the association of genetic, environmental and immune deregulation, which culminates in the development and progression of the inflammatory process. In an attempt to reverse colonic inflammation, endogenous systems involved in intestinal physiology are studied and the cholinergic system is fundamental for this process. In addition, this system has anti-inflammatory action in experimental models of IBD. Another important endogenous system in regulating the exacerbated inflammatory response in the gut is mediated by endocannabinoids, which play an important role in restoring bowel functionality after the onset of the inflammatory process. There are several reports in the literature showing the interconnection between the cannabinoid and cholinergic systems in different tissues. Considering that the activation of the cholinergic system stimulates the production of cannabinoid agonists in the intestine, our hypothesis is that the interaction between the muscarinic system and the cannabinoid in the control of intestinal inflammation is mediated by endogenous cannabinoids, since they are stimulated by the activation of muscarinic receptors.” “Burning mouth syndrome (BMS) is a neuropathic pain disorder associated with a burning sensation on oral mucosal surfaces with frequently reported xerostomia, dysgeusia and tingling or paraesthetic sensations. However, patients present no clinically evident causative lesions. The poor classification of the disorder has resulted in a diagnostic challenge, particularly for the clinician/dentist evaluating these individuals. Major research developments have been made in the BMS field in recent years to address this concern, principally in terms of the pathophysiological mechanisms underlying the disorder, in addition to therapeutic advancements. For the purpose of this review, an update on the pathophysiological mechanisms will be discussed from a neuropathic, immunological, hormonal and psychological perspective. This review will also focus on the many therapeutic strategies that have been explored for BMS, including antidepressants/antipsychotics, nonsteroidal anti-inflammatories, hormone replacement therapies, phytotherapeutic compounds and non-pharmacological interventions, overall highlighting the lack of controlled clinical studies to support the effectiveness of such therapeutic avenues. Particular focus is given to the
“Burning mouth syndrome (BMS) is a neuropathic pain disorder associated with a burning sensation on oral mucosal surfaces with frequently reported xerostomia, dysgeusia and tingling or paraesthetic sensations. However, patients present no clinically evident causative lesions. The poor classification of the disorder has resulted in a diagnostic challenge, particularly for the clinician/dentist evaluating these individuals. Major research developments have been made in the BMS field in recent years to address this concern, principally in terms of the pathophysiological mechanisms underlying the disorder, in addition to therapeutic advancements. For the purpose of this review, an update on the pathophysiological mechanisms will be discussed from a neuropathic, immunological, hormonal and psychological perspective. This review will also focus on the many therapeutic strategies that have been explored for BMS, including antidepressants/antipsychotics, nonsteroidal anti-inflammatories, hormone replacement therapies, phytotherapeutic compounds and non-pharmacological interventions, overall highlighting the lack of controlled clinical studies to support the effectiveness of such therapeutic avenues. Particular focus is given to the  “The number of patients using
“The number of patients using