
Most of the effects of cannabinoids are mediated by the well-characterized cannabinoid receptors, the cannabinoid type 1 receptor (CB1R) and cannabinoid type 2 receptor (CB2R). Even though CB1Rs are highly expressed in the central nervous system (CNS), the adverse central side effects and the development of tolerance resulting from CB1R activation may ultimately limit the clinical utility of CB1R agonists. In contrast to the ubiquitous presence of CB1Rs, CB2Rs are less commonly expressed in the healthy CNS but highly upregulated in glial cells under neuropathological conditions.
Experimental studies have provided robust evidence that CB2Rs seem to be involved in the modulation of different neurological disorders. In this paper, we summarize the current knowledge regarding the protective effects of CB2R activation against the development of neurological diseases and provide a perspective on the future of this field. A better understanding of the fundamental pharmacology of CB2R activation is essential for the development of clinical applications and the design of novel therapeutic strategies.”

 “Cannabinoids help in pain treatment through their action on CB1 and CB2 receptors.
“Cannabinoids help in pain treatment through their action on CB1 and CB2 receptors. “While activation of cannabinoid (CB2) receptors has been shown to be neuroprotective, no studies have examined whether this neuroprotection is directed at cerebral arterioles and no studies have examined whether activation of CB2 receptors can rescue cerebrovascular dysfunction during a chronic disease state such as type 1 diabetes (T1D).
“While activation of cannabinoid (CB2) receptors has been shown to be neuroprotective, no studies have examined whether this neuroprotection is directed at cerebral arterioles and no studies have examined whether activation of CB2 receptors can rescue cerebrovascular dysfunction during a chronic disease state such as type 1 diabetes (T1D).

 “Alcohol is a psychoactive substance highly used worldwide, whose harmful use might cause a broad range of mental and behavioural disorders. Underlying brain impact, the neuroinflammatory response induced by alcohol is recognised as a key contributing factor in the progression of other neuropathological processes, such as neurodegeneration. These sequels are determined by multiple factors, including age of exposure.
“Alcohol is a psychoactive substance highly used worldwide, whose harmful use might cause a broad range of mental and behavioural disorders. Underlying brain impact, the neuroinflammatory response induced by alcohol is recognised as a key contributing factor in the progression of other neuropathological processes, such as neurodegeneration. These sequels are determined by multiple factors, including age of exposure.
 “Cannabinoid CB2 receptor (CB2) agonists are potential analgesics void of psychotropic effects.
“Cannabinoid CB2 receptor (CB2) agonists are potential analgesics void of psychotropic effects. “Chronic ethanol abuse can lead to harmful consequences for the heart, resulting in systolic dysfunction, variability in the heart rate, arrhythmia, and cardiac remodelling. However, the precise molecular mechanism responsible for ethanol-induced cardiomyopathy is poorly understood. In this regard, the present study aimed to describe the RIP1/RIP3/MLKL-mediated necroptotic cell death that may be involved in ethanol-induced cardiomyopathy and characterize CBR-mediated effects on the signalling pathway and myocardial injury.
“Chronic ethanol abuse can lead to harmful consequences for the heart, resulting in systolic dysfunction, variability in the heart rate, arrhythmia, and cardiac remodelling. However, the precise molecular mechanism responsible for ethanol-induced cardiomyopathy is poorly understood. In this regard, the present study aimed to describe the RIP1/RIP3/MLKL-mediated necroptotic cell death that may be involved in ethanol-induced cardiomyopathy and characterize CBR-mediated effects on the signalling pathway and myocardial injury. “Cannabinoids (CBs), analgesic drugs used for thousands of years, were first found in Cannabis sativa, and the multiple CBs used medicinally, such as tetrahydrocannabinol (THC), cannabidiol (CBD) and dozens more, have complex structures. In addition to their production by plants, CBs are naturally present in the nerves and immune systems of humans and animals.
“Cannabinoids (CBs), analgesic drugs used for thousands of years, were first found in Cannabis sativa, and the multiple CBs used medicinally, such as tetrahydrocannabinol (THC), cannabidiol (CBD) and dozens more, have complex structures. In addition to their production by plants, CBs are naturally present in the nerves and immune systems of humans and animals.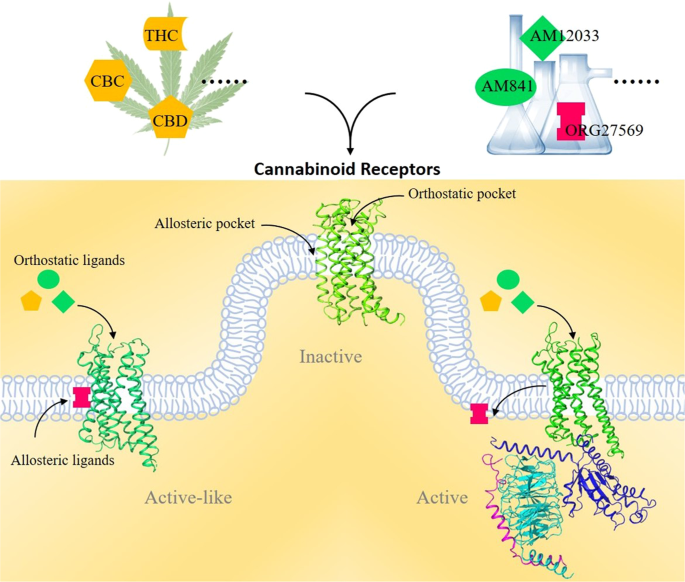
 “Like most modern molecular biology and natural product chemistry, understanding cannabinoid pharmacology centers around molecular interactions, in this case, between the cannabinoids and their putative targets, the G-protein coupled receptors (GPCRs) cannabinoid receptor 1 (CB1) and cannabinoid receptor 2 (CB2). Understanding the complex structure and interplay between the partners in this molecular dance is required to understand the mechanism of action of synthetic, endogenous, and phytochemical cannabinoids. This review, with 91 references, surveys our understanding of the structural biology of the cannabinoids and their target receptors including both a critical comparison of the extant crystal structures and the computationally derived homology models, as well as an in-depth discussion about the binding modes of the major cannabinoids. The aim is to assist in situating structural biochemists, synthetic chemists, and molecular biologists who are new to the field of cannabis research.”
“Like most modern molecular biology and natural product chemistry, understanding cannabinoid pharmacology centers around molecular interactions, in this case, between the cannabinoids and their putative targets, the G-protein coupled receptors (GPCRs) cannabinoid receptor 1 (CB1) and cannabinoid receptor 2 (CB2). Understanding the complex structure and interplay between the partners in this molecular dance is required to understand the mechanism of action of synthetic, endogenous, and phytochemical cannabinoids. This review, with 91 references, surveys our understanding of the structural biology of the cannabinoids and their target receptors including both a critical comparison of the extant crystal structures and the computationally derived homology models, as well as an in-depth discussion about the binding modes of the major cannabinoids. The aim is to assist in situating structural biochemists, synthetic chemists, and molecular biologists who are new to the field of cannabis research.”