 “Central pain after stroke due to brainstem infarction is very rare. Treatment is difficult and specific guidelines are lacking. This is the report of a 61-year-old female patient who, after a posterolateral left medulla oblongata insult with incomplete Wallenberg syndrome, subsequently developed a burning and tingling pain in the contralateral leg and a burning and shooting pain in the ipsilateral face in trigeminal branches 1 and 2. More than 3 years of therapy with amitriptyline, gabapentin, pregabalin and various grade II and III opioids was ineffective or showed intolerable side effects. The administration of tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio improved the pain situation and quality of life quickly and permanently. The encouraging results in the present case may suggest that treatment with medical cannabis should be considered in similar cases when standard therapies are insufficient.”
“Central pain after stroke due to brainstem infarction is very rare. Treatment is difficult and specific guidelines are lacking. This is the report of a 61-year-old female patient who, after a posterolateral left medulla oblongata insult with incomplete Wallenberg syndrome, subsequently developed a burning and tingling pain in the contralateral leg and a burning and shooting pain in the ipsilateral face in trigeminal branches 1 and 2. More than 3 years of therapy with amitriptyline, gabapentin, pregabalin and various grade II and III opioids was ineffective or showed intolerable side effects. The administration of tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio improved the pain situation and quality of life quickly and permanently. The encouraging results in the present case may suggest that treatment with medical cannabis should be considered in similar cases when standard therapies are insufficient.”
Tag Archives: THC
Effects of tetrahydrocannabinols on human oral cancer cell proliferation, apoptosis, autophagy, oxidative stress, and DNA damage
 “Cannabinoids, including delta-8- and delta-9-tetrahydrocannabinol (THC) have a palliative care impact and may therefore be beneficial against cancer.
“Cannabinoids, including delta-8- and delta-9-tetrahydrocannabinol (THC) have a palliative care impact and may therefore be beneficial against cancer.
The aim of this study was to investigate the effect of Δ9-THC and Δ8-THC on oral cancer cell behaviors.
Results: Both cannabinoids were found to decrease cell viability/proliferation by blocking the cell cycle progression from the S to the G2/M phase and enhancing their apoptosis and autophagy. Δ9-THC and Δ8-THC also suppressed the migration/invasion by inhibiting epithelial-mesenchymal transition markers, such as E-cadherin, in addition to decreasing reactive oxygen species (ROS) production and increasing glutathione (GSH) and the expression of mtMP. Δ9-THC and Δ8-THC also downregulated cyclin D1, p53, NOXA, PUMAα, and DRAM expressions but increased p21 and H2AX expression.
Conclusion: We demonstrated that cannabinoids (Δ9-THC and Δ8-THC) were able to decrease oral cancer cell growth through various mechanisms, including apoptosis, autophagy, and oxidative stress. These results suggest a potential use of these molecules as a therapy against oral cancer.”
https://pubmed.ncbi.nlm.nih.gov/34146926/
“Cannabinoids (Δ9-THC and Δ8-THC) decrease oral cancer cell viability/ proliferation.”
https://www.sciencedirect.com/science/article/abs/pii/S0003996921001631?via%3Dihub
A Phase 2 Randomised Clinical Trial Assessing the Tolerability of Two Different Ratios of Medicinal Cannabis in Patients With High Grade Gliomas
 “Background: Cannabis for cancer is very topical and, given the use of illicit cannabis preparations used in this vulnerable population, research investigating standardised, quality-assured medicinal cannabis is critical to inform clinicians and assist patient safety.
“Background: Cannabis for cancer is very topical and, given the use of illicit cannabis preparations used in this vulnerable population, research investigating standardised, quality-assured medicinal cannabis is critical to inform clinicians and assist patient safety.
Methods: A randomized trial involving adult patients diagnosed with a high-grade glioma, no history of substance abuse, liver or kidney damage or myocardial infarction were eligible for inclusion in a tolerability study on two different ratios of medicinal cannabis. Baseline screening of brain morphology, blood pathology, functional status, and cognition was conducted. A retrospective control group was used for comparison for secondary outcomes.
Results: Participants (n=88) were on average 53.3 years old. A paired t-test assessed the Functional Assessment of Cancer Therapy for Brain Cancer (FACT-Br) between groups from baseline to week 12 found that the 1:1 ratio favoured both physical (p=0.025) and functional (p=0.014) capacity and improved sleep (p=0.009). Analysis of changes from baseline to week 12 also found 11% of 61 participants had a reduction in disease, 34% were stable, 16% had slight enhancement, and 10% had progressive disease. No serious adverse events occurred. Side effects included dry mouth, tiredness at night, dizziness, drowsiness.
Conclusion: This study demonstrated that a single nightly dose of THC-containing medicinal cannabis was safe, had no serious adverse effects and was well tolerated in patients. Medicinal cannabis significantly improved sleep, functional wellbeing, and quality of life.”
https://pubmed.ncbi.nlm.nih.gov/34094937/
“From this study we have shown that a single nightly dose of THC-containing cannabis was well tolerated in patients in both groups with high-grade gliomas and significantly improved sleep, functional wellbeing and contentment with QoL in a sample of patients compared to baseline. From this trial, the 1:1 ratio has been identified as the preferred combination the moving forward to further trials. This study significantly informs MC product choice for ongoing studies into cannabis being a potential adjunct treatment option for this patient population.”
https://www.frontiersin.org/articles/10.3389/fonc.2021.649555/full
Prolonged Medical Cannabis Treatment is Associated With Quality of Life Improvement and Reduction of Analgesic Medication Consumption in Chronic Pain Patients
 “Introduction: Chronic non-cancer pain (CNCP) is one of the most prevalent indications for medical cannabis (MC) treatment globally. In this study, we investigated CNCP parameters in patients during prolonged MC treatment, and assessed the interrelation between CNCP parameters and the chemical composition of MC chemovar used.
“Introduction: Chronic non-cancer pain (CNCP) is one of the most prevalent indications for medical cannabis (MC) treatment globally. In this study, we investigated CNCP parameters in patients during prolonged MC treatment, and assessed the interrelation between CNCP parameters and the chemical composition of MC chemovar used.
Methods: A cross-sectional questionnaire-based study was performed in one-month intervals for the duration of six months. Subjects were adult patients licensed for MC treatment who also reported a diagnosis of CNCP by a physician. Data included self-reported questionnaires. MC treatment features included administration route, cultivator, cultivar name and monthly dose. Comparison statistics were used to evaluate differences between the abovementioned parameters and the monthly MC chemovar doses at each time point.
Results: 429, 150, 98, 71, 77 and 82 patients reported fully on their MC treatment regimens at six one-month intervals, respectively. Although pain intensities did not change during the study period, analgesic medication consumption rates decreased from 46 to 28% (p < 0.005) and good Quality of Life (QoL) rates increased from 49 to 62% (p < 0.05). These changes overlapped with increase in rates of (-)-Δ9–trans-tetrahydrocannabinol (THC) and α-pinene high dose consumption.
Conclusion: Even though we observed that pain intensities did not improve during the study, QoL did improve and the rate of analgesic medication consumption decreased alongside with increasing rates of high dose THC and α-pinene consumption. Understanding MC treatment composition may shed light on its long-term effects.”
“In this study, although pain intensities did not change under long-term MC treatment, analgesic medication consumption rates decreased and ‘better’ QoL rates increased. These changes coincided with the increased rates of patients’ consumption of high dose THC and α pinene. These results may shed light on the long-term beneficial effects of MC on CNCP.”
https://www.frontiersin.org/articles/10.3389/fphar.2021.613805/full
Therapeutic Prospects of Cannabinoids in the Immunomodulation of Prevalent Autoimmune Diseases
 “Cannabinoids such as ▵-9-THC and CBD can downregulate the immune response by modulating the endocannabinoid system. This modulation is relevant for the treatment of prevalent autoimmune diseases (ADs), such as multiple sclerosis (MS), systemic lupus erythematosus (SLE), diabetes mellitus type 1 (DMT1), and rheumatoid arthritis (RA). These conditions require new therapeutic options with fewer side effects for the control of the autoimmune response. Objective: to conduct a literature review of preclinical scientific evidence that supports further clinical investigations for the use of cannabinoids (natural or synthetic) as potential immunomodulators of the immune response in ADs.
“Cannabinoids such as ▵-9-THC and CBD can downregulate the immune response by modulating the endocannabinoid system. This modulation is relevant for the treatment of prevalent autoimmune diseases (ADs), such as multiple sclerosis (MS), systemic lupus erythematosus (SLE), diabetes mellitus type 1 (DMT1), and rheumatoid arthritis (RA). These conditions require new therapeutic options with fewer side effects for the control of the autoimmune response. Objective: to conduct a literature review of preclinical scientific evidence that supports further clinical investigations for the use of cannabinoids (natural or synthetic) as potential immunomodulators of the immune response in ADs.
Methodology: A systematic search was carried out in different databases using different MeSH terms, such as Cannabis sativa L., cannabinoids, immunomodulation, and ADs. Initially, 677 journal articles were found. After filtering by publication date (from 2000 to 2020 for SLE, DMT1, and RA; and 2010 to 2020 for MS) and removing the duplicate items, 200 articles were selected and analyzed by title and summary associated with the use of cannabinoids as immunomodulatory treatment for those diseases.
Results: Evidence of the immunomodulatory effect of cannabinoids in the diseases previously mentioned, but SLE that did not meet the search criteria, was summarized from 24 journal articles. CBD was found to be one of the main modulators of the immune response. This molecule decreased the number of Th1 and Th17 proinflammatory cells and the production of the proinflammatory cytokines, interleukin (IL)-1, IL-12, IL-17, interferon (IFN)-γ, and tumor necrosis factor alpha, in mouse models of MS and DMT1. Additionally, new synthetic cannabinoid-like molecules, with agonist or antagonist activity on CB1, CB2, TRPV1, PPAR-α, and PPAR-γ receptors, have shown anti-inflammatory properties in MS, DMT1, and RA.
Conclusion: Data from experimental animal models of AD showed that natural and synthetic cannabinoids downregulate inflammatory responses mediated by immune cells responsible for AD chronicity and progression. Although synthetic cannabinoid-like molecules were evaluated in just two clinical trials, they corroborated the potential use of cannabinoids to treat some ADs. Notwithstanding, new cannabinoid-based approaches are required to provide alternative treatments to patients affected by the large group of ADs.”
https://pubmed.ncbi.nlm.nih.gov/34030476/
https://www.liebertpub.com/doi/10.1089/can.2020.0183
Recovery from Traumatic Brain Injury Following Treatment with Δ9-Tetrahydrocannabinol Is Associated with Increased Expression of Granulocyte-Colony Stimulating Factor and Other Neurotrophic Factors
 “The hematopoietic cytokine granulocyte-colony stimulating factor (G-CSF) is well known to stimulate proliferation of blood stem/progenitor cells of the leukocyte lineage, but is also recognized as a neurotrophic factor involved in brain self-repair processes. G-CSF administration has been shown to promote recovery from experimental models of traumatic brain injury (TBI) and to modulate components of the endocannabinoid system (eCS). Conversely, Δ9-tetrahydrocannabinol (Δ9THC) treatment of normal mice has been shown to increase blood levels of G-CSF in the periphery.
“The hematopoietic cytokine granulocyte-colony stimulating factor (G-CSF) is well known to stimulate proliferation of blood stem/progenitor cells of the leukocyte lineage, but is also recognized as a neurotrophic factor involved in brain self-repair processes. G-CSF administration has been shown to promote recovery from experimental models of traumatic brain injury (TBI) and to modulate components of the endocannabinoid system (eCS). Conversely, Δ9-tetrahydrocannabinol (Δ9THC) treatment of normal mice has been shown to increase blood levels of G-CSF in the periphery.
Hypothesis: Administration of the phytocannabinoid Δ9THC will enhance brain repair following controlled cortical impact (CCI) by upregulating G-CSF and other neurotrophic factors (brain-derived neurotrophic factor [BDNF] and glial-derived neurotrophic factor [GDNF]) in brain regions.
Materials and Methods: C57BL/6J mice underwent CCI and were treated for 3 days with THC 3 mg/kg intraperitoneally. Motor function on a rotarod was recorded at baseline and 3, 7, and 14 days after CCI. Groups of mice were euthanized at 7 and 14 days. G-CSF, BDNF, and GDNF expression were measured at 7 and 14 days in cerebral cortex, striatum, and hippocampus on the side of the trauma.
Results: Δ9THC-treated mice ran on the rotarod longer than vehicle-treated mice and recovered to normal rotarod performance levels at 2 weeks. These mice, compared to vehicle-treated animals, exhibited significant upregulation of G-CSF as well as BDNF and GDNF in cerebral cortex, striatum, and hippocampus.
Conclusion: Administration of the phytocannabinoid Δ9THC promotes significant recovery from TBI and is associated with upregulation of brain G-CSF, BDNF, and GDNF, neurotrophic factors previously shown to mediate brain self-repair following TBI and stroke.”
Specific Compositions of Cannabis sativa Compounds Have Cytotoxic Activity and Inhibit Motility and Colony Formation of Human Glioblastoma Cells In Vitro
 “Glioblastoma multiforme (GBM) is the most lethal subtype of glioma. Cannabis sativa is used for the treatment of various medical conditions. Around 150 phytocannabinoids have been identified in C. sativa, among them Δ-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) that trigger GBM cell death. However, the optimal combinations of cannabis molecules for anti-GBM activity are unknown. Chemical composition was determined using high-performance liquid chromatography (HPLC) and gas chromatography mass spectrometry (GC/MS). Cytotoxic activity was determined by XTT and lactate dehydrogenase (LDH) assays and apoptosis and cell cycle by fluorescence-activated cell sorting (FACS). F-actin structures were observed by confocal microscopy, gene expression by quantitative PCR, and cell migration and invasion by scratch and transwell assays, respectively. Fractions of a high-THC cannabis strain extract had significant cytotoxic activity against GBM cell lines and glioma stem cells derived from tumor specimens. A standard mix (SM) of the active fractions F4 and F5 induced apoptosis and expression of endoplasmic reticulum (ER)-stress associated-genes. F4 and F5 inhibited cell migration and invasion, altered cell cytoskeletons, and inhibited colony formation in 2 and 3-dimensional models. Combinations of cannabis compounds exert cytotoxic, anti-proliferative, and anti-migratory effects and should be examined for efficacy on GBM in pre-clinical studies and clinical trials.”
“Glioblastoma multiforme (GBM) is the most lethal subtype of glioma. Cannabis sativa is used for the treatment of various medical conditions. Around 150 phytocannabinoids have been identified in C. sativa, among them Δ-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) that trigger GBM cell death. However, the optimal combinations of cannabis molecules for anti-GBM activity are unknown. Chemical composition was determined using high-performance liquid chromatography (HPLC) and gas chromatography mass spectrometry (GC/MS). Cytotoxic activity was determined by XTT and lactate dehydrogenase (LDH) assays and apoptosis and cell cycle by fluorescence-activated cell sorting (FACS). F-actin structures were observed by confocal microscopy, gene expression by quantitative PCR, and cell migration and invasion by scratch and transwell assays, respectively. Fractions of a high-THC cannabis strain extract had significant cytotoxic activity against GBM cell lines and glioma stem cells derived from tumor specimens. A standard mix (SM) of the active fractions F4 and F5 induced apoptosis and expression of endoplasmic reticulum (ER)-stress associated-genes. F4 and F5 inhibited cell migration and invasion, altered cell cytoskeletons, and inhibited colony formation in 2 and 3-dimensional models. Combinations of cannabis compounds exert cytotoxic, anti-proliferative, and anti-migratory effects and should be examined for efficacy on GBM in pre-clinical studies and clinical trials.”
“Glioblastoma multiforme (GBM) is the most frequent, invasive, and lethal subtype of glioma brain tumors. Cannabis is commonly used for medical treatment, and individual phytocannabinoids have been shown to trigger GBM cell death. However, cannabis contains hundreds of different compounds, and the optimal combinations of molecules with anti-GBM activity are unknown. Here, we identified fractions from a cannabis strain that substantially reduced human GBM cell viability and motility. The fractions also reduced the ability of GBM cells to form colonies in 2 and 3-dimensional models, suggesting that the cannabis treatments may have the potential for preventing the formation of GBM neurospheres associated with the high resistance to current therapies. Importantly, these compounds also induced cell death in glioma stem cells derived from tumor specimens. The effectiveness of the fractions and combinations of cannabis compounds should be examined in GBM pre-clinical studies and clinical trials.”
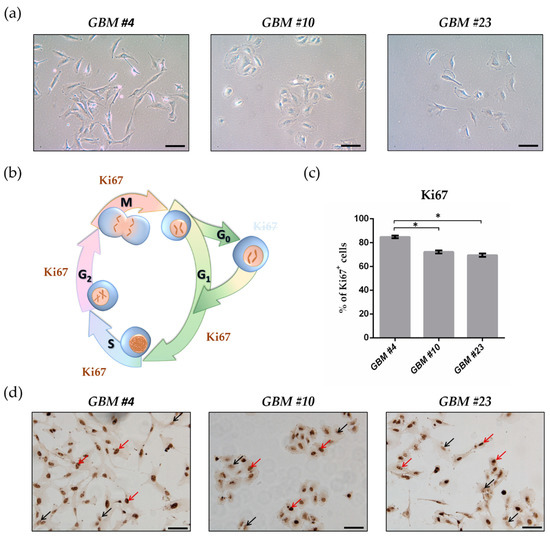
THC Reduces Ki67-Immunoreactive Cells Derived from Human Primary Glioblastoma in a GPR55-Dependent Manner

“Glioblastoma (GBM) is the most frequent malignant tumor of the central nervous system in humans with a median survival time of less than 15 months.
∆9-Tetrahydrocannabinol (THC) and cannabidiol (CBD) are the best-characterized components of Cannabis sativa plants with modulating effects on cannabinoid receptors 1 and 2 (CB1 and CB2) and on orphan receptors such as GPR18 or GPR55. Previous studies have demonstrated anti-tumorigenic effects of THC and CBD in several tumor entities including GBM, mostly mediated via CB1 or CB2.
In this study, we investigated the non-CB1/CB2 effects of THC on the cell cycle of GBM cells isolated from human tumor samples.
Cell cycle entry was measured after 24 h upon exposure by immunocytochemical analysis of Ki67 as proliferation marker. The Ki67-reducing effect of THC was abolished in the presence of CBD, whereas CBD alone did not cause any changes. To identify the responsible receptor for THC effects, we first characterized the cells regarding their expression of different cannabinoid receptors: CB1, CB2, GPR18, and GPR55. Secondly, the receptors were pharmacologically blocked by application of their selective antagonists AM281, AM630, O-1918, and CID16020046 (CID), respectively. All examined cells expressed the receptors, but only in presence of the GPR55 antagonist CID was the THC effect diminished. Stimulation with the GPR55 agonist lysophosphatidylinositol (LPI) revealed similar effects as obtained for THC. The LPI effects were also inhibited by CBD and CID, confirming a participation of GPR55 and suggesting its involvement in modifying the cell cycle of patient-derived GBM cells.”
https://pubmed.ncbi.nlm.nih.gov/33802282/
https://www.mdpi.com/2072-6694/13/5/1064
Efficacy of cannabinoids against glioblastoma multiforme: A systematic review

“INTRODUCTION
: The increased incidence of Glioblastoma Multiforme, the most aggressive and most common primary brain tumour, is evident worldwide. Survival rates are reaching only 15 months due to its high recurrence and resistance to current combination therapies including oncotomy, radiotherapy and chemotherapy. Light has been shed in the recent years on the anticancer properties of cannabinoids from Cannabis sativa.
OBJECTIVE
: To determine whether cannabinoids alone or in combination with radiotherapy and/or chemotherapy inhibit tumour progression, induce cancer cell death, inhibit metastasis and invasiveness and the mechanisms that underlie these actions.
METHOD
: PubMed and Web of Science were used for a systemic search to find studies on the anticancer effects of natural cannabinoids on glioma cancer cells in vitro and/or in vivo.
RESULTS
: A total of 302 papers were identified, of which 14 studies were found to fit the inclusion criteria. 5 studies were conducted in vitro, 2 in vivo and 7 were both in vivo and in vitro. 3 studies examined the efficacy of CBD, THC and TMZ, 1 study examined CBD and radiation, 2 studies examined efficacy of THC only and 3 studies examined the efficacy of CBD only. 1 study examined the efficacy of CBD, THC and radiotherapy, 2 studies examined the combination of CBD and THC and 2 more studies examined the efficacy of CBD and TMZ.
CONCLUSION
: The evidence in this systematic review leads to the conclusion that cannabinoids possess anticancer potencies against glioma cells, however this effect varies with the combinations and dosages used. Studies so far were conducted on cells in culture and on mice as well as a small number of studies that were conducted on humans. Hence in order to have more accurate results, higher quality studies mainly including human clinical trials with larger sample sizes are necessitated urgently for GBM treatment.”
HTTPS://WWW.SCIENCEDIRECT.COM/SCIENCE/ARTICLE/ABS/PII/S0944711321000751
Unveiling the mechanism of action behind the anti-cancer properties of cannabinoids in ER + breast cancer cells: impact on aromatase and steroid receptors
 “Breast cancer is the leading cause of cancer-related death in women worldwide. In the last years, cannabinoids have gained attention in the clinical setting and clinical trials with cannabinoid-based preparations are underway. However, contradictory anti-tumour properties have also been reported. Thus, the elucidation of the molecular mechanisms behind their anti-tumour efficacy is crucial to better understand its therapeutic potential.
“Breast cancer is the leading cause of cancer-related death in women worldwide. In the last years, cannabinoids have gained attention in the clinical setting and clinical trials with cannabinoid-based preparations are underway. However, contradictory anti-tumour properties have also been reported. Thus, the elucidation of the molecular mechanisms behind their anti-tumour efficacy is crucial to better understand its therapeutic potential.
Considering this, our work aims to clarify the molecular mechanisms underlying the anti-cancer properties of the endocannabinoid anandamide (AEA) and of the phytocannabinoids, cannabidiol (CBD) and Δ9-tetrahydrocannabinol (THC), in estrogen receptor-positive (ER+) breast cancer cells that overexpress aromatase (MCF-7aro). Their in vitro effects on cell proliferation, cell death and activity/expression of aromatase, ERα, ERβ and AR were investigated.
Our results demonstrated that cannabinoids disrupted MCF-7aro cell cycle progression. Unlike AEA and THC that induced apoptosis, CBD triggered autophagy to promote apoptotic cell death. Interestingly, all cannabinoids reduced aromatase and ERα expression levels in cells. On the other hand, AEA and CBD not only exhibited high anti-aromatase activity but also induced up-regulation of ERβ. Therefore, all cannabinoids, albeit by different actions, target aromatase and ERs, impairing, in that way, the growth of ER+ breast cancer cells, which is dependent on estrogen signalling.
As aromatase and ERs are key targets for ER+ breast cancer treatment, cannabinoids can be considered as potential and attractive therapeutic compounds for this type of cancer, being CBD the most promising one. Thus, from an in vitro perspective, this work may contribute to the growing mass of evidence of cannabinoids and cannabinoids-based medicines as potential anti-cancer drugs.”
https://pubmed.ncbi.nlm.nih.gov/33722705/
“AEA and THC induce apoptosis in ER+ breast cancer cells, while CBD trigger autophagy to promote apoptosis. AEA, THC and CBD impair growth of ER+ breast cancer cells, by disrupting cycle progression. AEA, THC and CBD affect aromatase and ERα expression levels in ER+ breast cancer cells. AEA and CBD strongly inhibited aromatase activity and up-regulated ERβ levels. Cannabinoids are considered potential therapeutic compounds for ER+ breast cancer, being CBD the most promising one.”
https://www.sciencedirect.com/science/article/abs/pii/S0960076021000698?via%3Dihub
