 “Alzheimer’s Dementia (AD) is a devastating neurodegenerative disease that affects approximately 17% of people aged 75-84. Neuropsychiatric symptoms (NPS) such as delusions, agitation, anxiety, and hallucinations are present in up to 95% of patients in all stages of dementia. To date, any approved and effective pharmacological interventions for the treatment of NPS are still not available.
“Alzheimer’s Dementia (AD) is a devastating neurodegenerative disease that affects approximately 17% of people aged 75-84. Neuropsychiatric symptoms (NPS) such as delusions, agitation, anxiety, and hallucinations are present in up to 95% of patients in all stages of dementia. To date, any approved and effective pharmacological interventions for the treatment of NPS are still not available.
We describe a clinical case of a female patient diagnosed with AD with continuous cognitive decline and dementia-related behavioral symptoms. Between 2008 and 2019, the patient was examined half-yearly at the memory clinic of the Medical University of Innsbruck. At each visit, cognitive state and pharmacological treatment were evaluated. In addition, NPs were assessed by using the neuropsychiatric inventory (NPI). In 2018, the patient progressed to severe AD stage and presented with progressive NPs (anxiety, suspected delusions, agitation, aggressive behavior, and suspected pain due to long immobility).
Consequently, off-label treatment with low-dose dronabinol was initiated, which facilitated a reduction of psychopharmacological treatment from six to three psychotropics. At the same time, the patient’s emotional state improved, while disruptive behavior, aggression, and sedation decreased significantly. This case report underpins the need for randomized, controlled trials to explore the effect of cannabinoid receptor agonists on behavioral and psychological symptoms in patients with severe AD.”
https://pubmed.ncbi.nlm.nih.gov/32477187/
“Cannabinoids have a distinct pharmacologic profile that may offer an alternative pharmacologic approach to antipsychotics and sedatives for treating NPs in patients with AD. In addition, the beneficial effect on appetite and pain may significantly improve quality of life of AD-patients and their caregivers.”
https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00413/full

 “Cannabis (Cannabis sativa L.) is a complex, polymorphic plant species, which produces a vast array of bioactive metabolites, the two major chemical groups being cannabinoids and terpenoids. Nonetheless, the psychoactive cannabinoid tetrahydrocannabinol (Δ 9 -THC) and the non-psychoactive cannabidiol (CBD), are the two major cannabinoids that have monopolized the research interest.
“Cannabis (Cannabis sativa L.) is a complex, polymorphic plant species, which produces a vast array of bioactive metabolites, the two major chemical groups being cannabinoids and terpenoids. Nonetheless, the psychoactive cannabinoid tetrahydrocannabinol (Δ 9 -THC) and the non-psychoactive cannabidiol (CBD), are the two major cannabinoids that have monopolized the research interest.
 “Multiple sclerosis (MS) is an autoimmune demyelinating disease of the central nervous system, affecting ambulation even in people with only mild neurological signs. Patients with MS frequently experience spasticity, which contributes significantly to impair their motor functions, including ambulation, owing to muscle stiffness, spasms, and pain.
“Multiple sclerosis (MS) is an autoimmune demyelinating disease of the central nervous system, affecting ambulation even in people with only mild neurological signs. Patients with MS frequently experience spasticity, which contributes significantly to impair their motor functions, including ambulation, owing to muscle stiffness, spasms, and pain. “Few models exist that can control for placebo and expectancy effects commonly observed in clinical trials measuring ‘
“Few models exist that can control for placebo and expectancy effects commonly observed in clinical trials measuring ‘ “While natural Δ9-tetrahidrocannabinol (Δ9THC),
“While natural Δ9-tetrahidrocannabinol (Δ9THC),  “An emerging area of preclinical research has investigated whether drug use in parents prior to conception influences drug responsivity in their offspring.
“An emerging area of preclinical research has investigated whether drug use in parents prior to conception influences drug responsivity in their offspring. “Cannabis sativa and its principal components, Δ9-tetrahydrocannabinol (Δ9-THC) and
“Cannabis sativa and its principal components, Δ9-tetrahydrocannabinol (Δ9-THC) and  “To examine acute and residual mood and cognitive performance in young adult regular
“To examine acute and residual mood and cognitive performance in young adult regular  “Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.
“Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.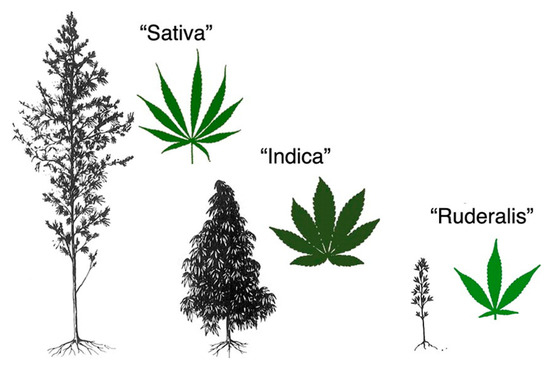
 “Borderline Personality Disorder (BPD) is a chronic debilitating psychiatric disorder characterized mainly by emotional instability, chaotic interpersonal relationships, cognitive disturbance (e.g. dissociation and suicidal thoughts) and maladaptive behaviors. BPD has a high rate of comorbidity with other mental disorders and high burden on society.
“Borderline Personality Disorder (BPD) is a chronic debilitating psychiatric disorder characterized mainly by emotional instability, chaotic interpersonal relationships, cognitive disturbance (e.g. dissociation and suicidal thoughts) and maladaptive behaviors. BPD has a high rate of comorbidity with other mental disorders and high burden on society.