
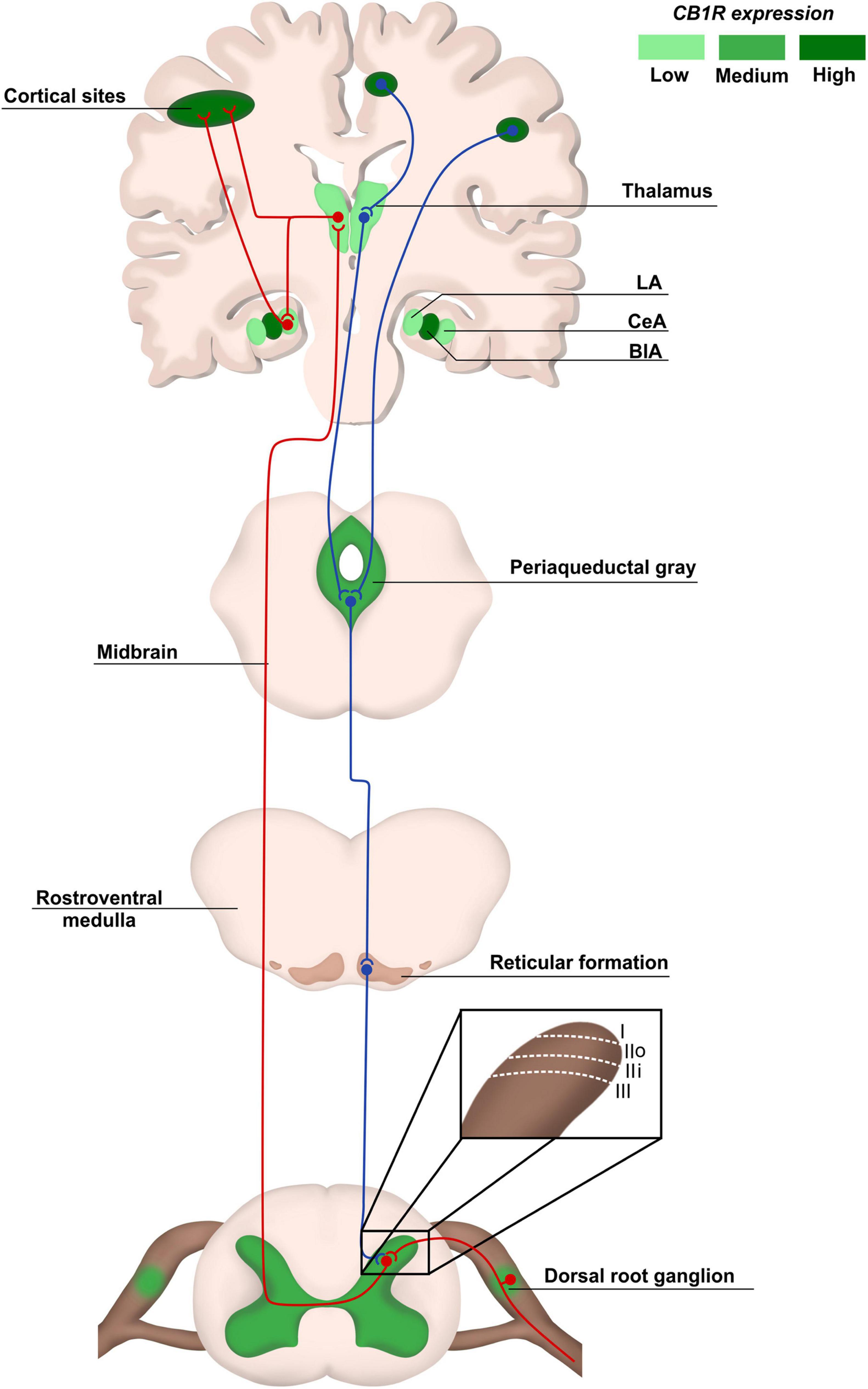
“Cannabinoid-based therapies offer a safer, non-opioid alternative for the management of chronic pain. While most studies focus on the analgesic potential of the main psychoactive component of marijuana, Δ9-tetrahydrocannabinol, fewer studies have investigated the role of the non-psychoactive component, cannabidiol (CBD). CBD has been purported to have analgesic, anti-inflammatory, anticonvulsant, and anxiolytic effects. In addition to having actions at both cannabinoid receptors (CB1 and CB2 ), CBD has been shown to interact with both the transient receptor potential vanilloid-1 (TRPV1) and serotonergic (5-HT) receptors. Clinically, CBD’s lack of psychoactivity and decreased abuse liability make it an appealing pharmacotherapeutic for the management of chronic pain. Therefore, the purpose of the current study was to determine whether CBD sex- or dose-dependently reverses antinociception in an acute model of thermal pain and/or mechanical allodynia in a model of cisplatin-induced chronic neuropathic pain. Furthermore, we observed the degree to which CB1 , CB2 , 5-HT, and TRPV1 receptors may be mediating these anti-allodynic responses. Male and female wild-type mice were assessed for either the anti-allodynic effects of 0, 1, 3, 10, and 30 mg/kg CBD in a cisplatin-induced model of neuropathic pain or the antinociceptive effects of 0, 1, 3, 10, 30, and 100 mg/kg CBD in a model of acute thermal (tail-flick) pain 60 minutes following CBD administration. To determine the relative contributions of each receptor subtype in mediating the anti-allodynic effects of CBD, male and female mice were pretreated with either: vehicle, the CB1 inverse agonist SR141716A (10 mg/kg), the CB2 antagonist SR144528 (10 mg/kg), the TRPV1 antagonist capsazepine (10 mg/kg), or the 5-HT2 antagonist methysergide (4 mg/kg) 30 minutes prior to treatment with CBD. Mice were assessed for the effects of the pretreatment alone and in combination with CBD. CBD at a dose of 3 mg/kg was able to partially reverse cisplatin-induced allodynia in male and female mice, while doses of 10 and 30 mg/kg resulted in nearly complete reversal. Our preliminary findings showed that the anti-allodynic effects of 30 mg/kg CBD were completely blocked following pretreatment with SR141716A and SR144528, and partially blocked by capsazepine in both male and female mice. Interestingly, pretreatment with methysergide partially attenuated the anti-allodynic effects of CBD in females alone. In contrast, CBD (0-100 mg/kg) failed to induce antinociception on the tail-flick assay. CBD did induce mild hypothermia with males showing a greater degree of CBD-mediated hypothermia than female mice. Taken together, these findings suggest that CBD may be a more effective treatment option for the management of chronic pain. This study highlights the therapeutic potential of CBD in a model of neuropathic pain and suggests that these effects may have clinical implications for the use of cannabinoids in chronic pain management.”
https://pubmed.ncbi.nlm.nih.gov/35560789/
https://faseb.onlinelibrary.wiley.com/doi/10.1096/fasebj.2022.36.S1.R5197


 “Background:
“Background:  “Human immunodeficiency virus (HIV) infection and antiretroviral therapy can independently induce HIV-associated neuropathic pain (HIV-NP).
“Human immunodeficiency virus (HIV) infection and antiretroviral therapy can independently induce HIV-associated neuropathic pain (HIV-NP). “Many people with MS (pwMS) use unregulated cannabis or cannabis products to treat the symptoms associated with the disease. In line with this, Sativex, a synthetic combination of cannabidiol (CBD) and Δ9-tetrahydrocannabinol (Δ9-THC) has been approved to treat symptoms of spasticity.
“Many people with MS (pwMS) use unregulated cannabis or cannabis products to treat the symptoms associated with the disease. In line with this, Sativex, a synthetic combination of cannabidiol (CBD) and Δ9-tetrahydrocannabinol (Δ9-THC) has been approved to treat symptoms of spasticity.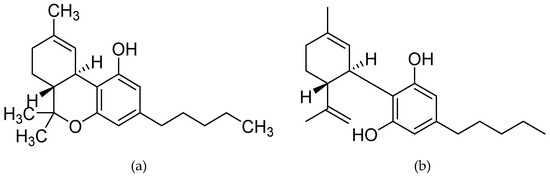
 “Recent studies have shown that cannabidiol (CBD) could have a great therapeutic potential for treating disorders such as chronic pain and anxiety. In the target article, the authors propose that CBD modulates serotonergic transmission and reverses allodynia and anxiety-like behaviour in a rat model of neuropathic pain. Furthermore, this study shows an antinociceptive effect mediated by TRPV1 and partially by 5-HT1A receptors, as well as an anxiolytic effect mediated by 5-HT1A receptors.”
“Recent studies have shown that cannabidiol (CBD) could have a great therapeutic potential for treating disorders such as chronic pain and anxiety. In the target article, the authors propose that CBD modulates serotonergic transmission and reverses allodynia and anxiety-like behaviour in a rat model of neuropathic pain. Furthermore, this study shows an antinociceptive effect mediated by TRPV1 and partially by 5-HT1A receptors, as well as an anxiolytic effect mediated by 5-HT1A receptors.” “Diabetes is a chronic disease associated with a high number of complications such as peripheral neuropathy, which causes sensorial disturbances and may lead to the development of diabetic neuropathic pain (DNP). The current treatment for DNP is just palliative and the drugs may cause severe adverse effects, leading to discontinuation of treatment. Thus, new therapeutic targets need to be urgently investigated.
“Diabetes is a chronic disease associated with a high number of complications such as peripheral neuropathy, which causes sensorial disturbances and may lead to the development of diabetic neuropathic pain (DNP). The current treatment for DNP is just palliative and the drugs may cause severe adverse effects, leading to discontinuation of treatment. Thus, new therapeutic targets need to be urgently investigated. “Cannabinoid CB2 receptor (CB2) agonists are potential analgesics void of psychotropic effects.
“Cannabinoid CB2 receptor (CB2) agonists are potential analgesics void of psychotropic effects. “Few models exist that can control for placebo and expectancy effects commonly observed in clinical trials measuring ‘
“Few models exist that can control for placebo and expectancy effects commonly observed in clinical trials measuring ‘