 “Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
“Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
Like Δ9-tetrahydrocannabinol (Δ9-THC), the most well-studied cannabinoid, CBD decreased lung inflammation in a murine model of acute lung injury potentially through the inhibition of proinflammatory cytokine production by immune cells and suppressing exuberant immune responses. CBD can inhibit the production of proinflammatory cytokines like interleukin (IL)-2, IL-6, IL-1α and β, interferon gamma, inducible protein-10, monocyte chemoattractant protein-1, macrophage inflammatory protein-1α, and tumor necrosis factor-α that have been associated with SARS-CoV2 induced multi-organ pathology and mortality. In a murine model of chronic asthma, CBD reduced proinflammatory cytokine production, airway inflammation and fibrosis. Moreover, CBD can effectively inhibit the JAK-STAT pathway including the production and action of type I interferons without leading to addiction, alterations in heart rate or blood pressure and adverse effects on the gastrointestinal tract and cognition. In simian immunodeficiency virus (SIV)-infected rhesus macaques (RMs), we reported THC mediated attenuation of IFN stimulated gene expression in the intestine. Similar to CBD, chronic THC administration blocked inflammation induced fibrosis in lymph nodes of chronically SIV-infected RMs. Unlike THC, CBD has a high margin of safety and is well tolerated pharmacologically even after treatments of up to 1500 mg/day for two weeks in both animals and humans, which suggests its feasibility to reduce SARS-CoV2 induced lung inflammation/pathology and disease severity.
The many uncertainties associated with the COVID-19 pandemic such as status of the economy, employment and loss of connection can fuel depression, fear and anxiety. CBD has shown promise as an alternative therapy for the clinical management of anxiety disorders. Based on its anxiolytic and anti-depressant properties, it has been suggested that CBD could be used to improve the mental and somatic health of patients suffering from anxiety and emotional stress after recovering from Ebola disease. Like Ebola, patients recovering from COVID-19 may experience various psychological and social stressors that may be triggered by residual chronic inflammation and autoimmune reactions. Therefore, randomized clinical trials to test the efficacy of CBD on alleviating anxiety and fear associated with COVID-19 infection and its consequences on people’s physical, social and psychological well-being may be beneficial in the future. Additionally, severely ill COVID-19 patients exhibited neurological symptoms like cerebrovascular disease, headache and disturbed consciousness (Reviewed in. Brain edema, neuronal degeneration and presence of SARS-CoV2 in the cerebrospinal fluid (CSF) were confirmed at autopsy. Therefore, longitudinal CSF sampling using non-human primate (NHP) studies may help clarify whether and when SARS-CoV2 invades the brain, and if this happens, does it result in neuroinflammation and more importantly, whether cannabinoids can modulate these events.
Being a negative allosteric modulator of the cannabinoid receptor-1, CBD can counter the psychotropic effects of THC when co-administered with THC. Although Remdesivir reduced the mortality rate of seriously ill COVID-19 patients needing invasive ventilation, similar studies in rhesus macaques revealed minimal subpleural inflammatory cellular infiltrates in the lungs of clinically recovered Remdesivir treated RMs at necropsy. This suggests persistence of inflammation and may partly explain the 20–30% reduction in lung function in COVID-19 patients after recovery, which if left unresolved may lead to pulmonary fibrosis. Collectively, these findings support the investigation of cannabinoids as a plausible option to be added as an adjunct to Remdesivir or any new antivirals on SARS-CoV2 induced lung inflammation.”
https://www.ncbi.nlm.nih.gov/pubmed/32360437
https://www.sciencedirect.com/science/article/pii/S0889159120307078?via%3Dihub
“Cannabis Indica speeds up Recovery from Coronavirus” https://www.researchgate.net/publication/339746853_Cannabis_Indica_speeds_up_Recovery_from_Coronavirus

 “Autism spectrum disorder (ASD) is a complex neurodevelopmental disorder with a multifactorial etiology. Latest researches are raising the hypothesis of a link between the onset of the main behavioral symptoms of ASD and the chronic neuroinflammatory condition of the autistic brain; increasing evidence of this connection is shedding light on new possible players in the pathogenesis of ASD.
“Autism spectrum disorder (ASD) is a complex neurodevelopmental disorder with a multifactorial etiology. Latest researches are raising the hypothesis of a link between the onset of the main behavioral symptoms of ASD and the chronic neuroinflammatory condition of the autistic brain; increasing evidence of this connection is shedding light on new possible players in the pathogenesis of ASD.
 “This article provides a concise overview of how cannabinoids and the endocannabinoid system (ECS) have significant implications for the prevention and treatment of metabolic syndrome (MetS) and for the treatment of cardiovascular disorders, including cardiac fibrosis.
“This article provides a concise overview of how cannabinoids and the endocannabinoid system (ECS) have significant implications for the prevention and treatment of metabolic syndrome (MetS) and for the treatment of cardiovascular disorders, including cardiac fibrosis. “Alzheimer’s disease (AD) is a multifactorial neurodegenerative disorder linked to various converging toxic mechanisms. Evidence suggests that hyperglycemia induces oxidative stress, mitochondrial dysfunction, inflammation and excitotoxicity, all of which play important roles in the onset and progression of AD pathogenesis.
“Alzheimer’s disease (AD) is a multifactorial neurodegenerative disorder linked to various converging toxic mechanisms. Evidence suggests that hyperglycemia induces oxidative stress, mitochondrial dysfunction, inflammation and excitotoxicity, all of which play important roles in the onset and progression of AD pathogenesis. “Resting-state (rs) network dysfunction is a contributing factor to treatment resistance in epilepsy. In treatment-resistant epilepsy (TRE), pharmacological and nonpharmacological therapies have been shown to improve such dysfunction.
“Resting-state (rs) network dysfunction is a contributing factor to treatment resistance in epilepsy. In treatment-resistant epilepsy (TRE), pharmacological and nonpharmacological therapies have been shown to improve such dysfunction. “The Cannabis plant contains numerous components, including cannabinoids and other active molecules. The phyto-cannabinoid activity is mediated by the endocannabinoid system. Cannabinoids affect the nervous system and play significant roles in the regulation of the immune system.
“The Cannabis plant contains numerous components, including cannabinoids and other active molecules. The phyto-cannabinoid activity is mediated by the endocannabinoid system. Cannabinoids affect the nervous system and play significant roles in the regulation of the immune system.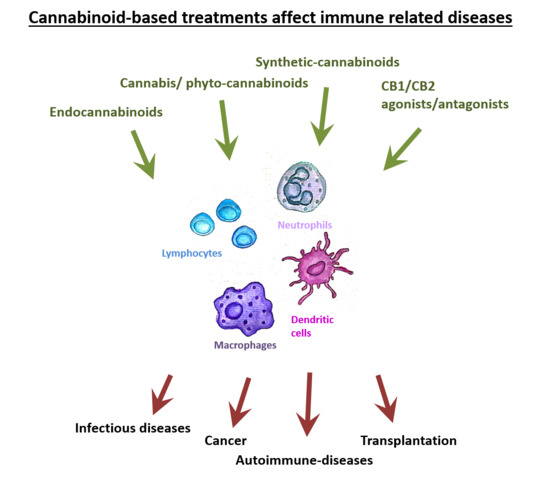
 “Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
“Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
 “Cannabis sativa produces hundreds of phytocannabinoids and terpenes.
“Cannabis sativa produces hundreds of phytocannabinoids and terpenes. “Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
“Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
 “Cannabis sativa L. (C. sativa) contains an array of plant-derived (phyto)
“Cannabis sativa L. (C. sativa) contains an array of plant-derived (phyto)