 “Cannabis sativa, commonly known as marijuana, contains a pool of secondary plant metabolites with therapeutic effects.
“Cannabis sativa, commonly known as marijuana, contains a pool of secondary plant metabolites with therapeutic effects.
Besides Δ9-tetrahydrocannabinol that is the principal psychoactive constituent of Cannabis, cannabidiol (CBD) is the most abundant nonpsychoactive phytocannabinoid and may represent a prototype for anti-inflammatory drug development for human pathologies where both the inflammation and oxidative stress (OS) play an important role to their etiology and progression.
To this regard, Alzheimer’s disease (AD), Parkinson’s disease (PD), the most common neurodegenerative disorders, are characterized by extensive oxidative damage to different biological substrates that can cause cell death by different pathways. Most cases of neurodegenerative diseases have a complex etiology with a variety of factors contributing to the progression of the neurodegenerative processes; therefore, promising treatment strategies should simultaneously target multiple substrates in order to stop and/or slow down the neurodegeneration.
In this context, CBD, which interacts with the eCB system, but has also cannabinoid receptor-independent mechanism, might be a good candidate as a prototype for anti-oxidant drug development for the major neurodegenerative disorders, such as PD and AD. This review summarizes the multiple molecular pathways that underlie the positive effects of CBD, which may have a considerable impact on the progression of the major neurodegenerative disorders.”
https://www.ncbi.nlm.nih.gov/pubmed/32210795
“The present review provided evidence that the nonpsychoactive phytocannabinoids CBD could be a potential pharmacological tool for the treatment of neurodegenerative disorders; its excellent safety and tolerability profile in clinical studies renders it a promising therapeutic agent.
The molecular mechanisms associated with CBD’s improvement in PD and AD are likely multifaceted, and although CBD may act on different molecular targets all the beneficial effects are in some extent linked to its antioxidant and anti-inflammatory profile, as observed in in vitro and in vivo studies. Therefore, this review describes evidence to prove the therapeutical efficacy of CBD in patients affected by neurodegenerative disorders and promotes further research in order to better elucidate the molecular pathways involved in the therapeutic potential of CBD.”
https://www.frontiersin.org/articles/10.3389/fphar.2020.00124/full
 “Parkinson’s Disease (PD) is currently the most rapid growing neurodegenerative disease and over the past generation, its global burden has more than doubled. The onset of PD can arise due to environmental, sporadic or genetic factors. Nevertheless, most PD cases have an unknown etiology.
“Parkinson’s Disease (PD) is currently the most rapid growing neurodegenerative disease and over the past generation, its global burden has more than doubled. The onset of PD can arise due to environmental, sporadic or genetic factors. Nevertheless, most PD cases have an unknown etiology.
 “Alcohol use disorders affect millions of people worldwide and there is growing evidence that excessive alcohol intake causes severe damage to the brain of both humans and animals.
“Alcohol use disorders affect millions of people worldwide and there is growing evidence that excessive alcohol intake causes severe damage to the brain of both humans and animals. “Cannabidiol (CBD) and cannabigerol (CBG) are Cannabis sativa terpenophenols.
“Cannabidiol (CBD) and cannabigerol (CBG) are Cannabis sativa terpenophenols.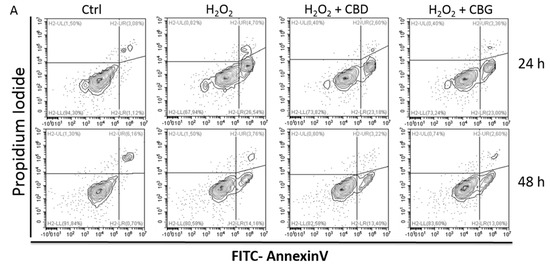
 “In this study cannabidiol (CBD) was administered orally to determine its effects and mechanisms in the experimental autoimmune encephalomyelitis (EAE) model of multiple sclerosis (MS). We hypothesized that 75 mg/kg of oral CBD given for 5 days after initiation of disease would reduce EAE severity through suppression of either the early peripheral immune or late neuroimmune response.
“In this study cannabidiol (CBD) was administered orally to determine its effects and mechanisms in the experimental autoimmune encephalomyelitis (EAE) model of multiple sclerosis (MS). We hypothesized that 75 mg/kg of oral CBD given for 5 days after initiation of disease would reduce EAE severity through suppression of either the early peripheral immune or late neuroimmune response.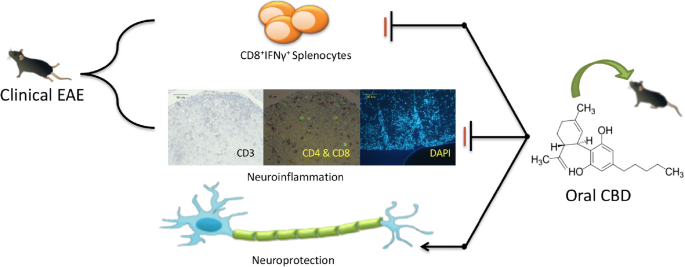
 “The antioxidant and CB2 receptor agonist properties of Δ9-tetrahydrocannabivarin (Δ9-THCV) afforded neuroprotection in experimental Parkinson’s disease (PD), whereas its CB1 receptor antagonist profile at doses lower than 5 mg/kg caused anti-hypokinetic effects.
“The antioxidant and CB2 receptor agonist properties of Δ9-tetrahydrocannabivarin (Δ9-THCV) afforded neuroprotection in experimental Parkinson’s disease (PD), whereas its CB1 receptor antagonist profile at doses lower than 5 mg/kg caused anti-hypokinetic effects. “Cannabis use in the management of musculoskeletal diseases has gained advocacy since several states have legalized its recreational use.
“Cannabis use in the management of musculoskeletal diseases has gained advocacy since several states have legalized its recreational use. “The societal burden of ischemic stroke suggests a need for additional therapeutic categories in stroke prevention.
“The societal burden of ischemic stroke suggests a need for additional therapeutic categories in stroke prevention. “Endocannabinoid system activity contributes to the homeostatic defense against aging and thus may counteract the progression of brain aging.
“Endocannabinoid system activity contributes to the homeostatic defense against aging and thus may counteract the progression of brain aging. “Medicinal use of
“Medicinal use of  “Cannabis sativa, commonly known as marijuana, contains a pool of secondary plant metabolites with therapeutic effects.
“Cannabis sativa, commonly known as marijuana, contains a pool of secondary plant metabolites with therapeutic effects.