 “Pharmaceutically purified oral cannabidiol (CBD) has been recently approved by the US Food and Drug Administration and European Medicines Agency as treatment of seizures associated with Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS), which are severe and difficult-to-treat developmental and epileptic encephalopathies with onset in early childhood.
“Pharmaceutically purified oral cannabidiol (CBD) has been recently approved by the US Food and Drug Administration and European Medicines Agency as treatment of seizures associated with Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS), which are severe and difficult-to-treat developmental and epileptic encephalopathies with onset in early childhood.
Areas covered: This review will critically review the pharmacokinetic properties of CBD, the interactions with antiseizure and non-antiseizure medications, and the main tolerability and safety issues to provide guidance for its use in everyday practice.
Expert opinion: CBD is metabolized in the liver and can influence the activity of enzymes involved in drug metabolism. The best characterized drug-drug interaction is between CBD and clobazam. The most common adverse events include somnolence, gastrointestinal discomfort and increase in serum transaminases.
High-grade purified CBD oral solution represents an effective therapeutic option in patients with DS and LGS.
The findings cannot be extrapolated to other cannabis-based products, synthetic cannabinoids for medicinal use and non-medicinal cannabis and CBD derivatives.”
https://pubmed.ncbi.nlm.nih.gov/33026899/
“Pharmaceutically purified oral cannabidiol (CBD) is approved for treatment of seizures associated with Dravet syndrome and Lennox-Gastaut syndrome.”
https://www.tandfonline.com/doi/abs/10.1080/14737175.2021.1834383?journalCode=iern20

 “Background/objectives: Use of cannabis is increasing in a variety of populations in the United States; however, few investigations about how and for what reasons cannabis is used in older populations exist.
“Background/objectives: Use of cannabis is increasing in a variety of populations in the United States; however, few investigations about how and for what reasons cannabis is used in older populations exist. “Rett syndrome (RTT) is a rare neurologic disorder, characterized by severe behavioural and physiological symptoms. RTT is caused by mutations in the MECP2 gene in about 95% of cases and to date no cure is available.
“Rett syndrome (RTT) is a rare neurologic disorder, characterized by severe behavioural and physiological symptoms. RTT is caused by mutations in the MECP2 gene in about 95% of cases and to date no cure is available. “Providers need to be better equipped to discuss medical cannabis with patients even if they are not willing to prescribe it. The oncology community would be well served to ensure that providers are aware of existing cannabis research and are able to incorporate it into their communications with patients instead of leaving patients to figure out medical cannabis on their own.”
“Providers need to be better equipped to discuss medical cannabis with patients even if they are not willing to prescribe it. The oncology community would be well served to ensure that providers are aware of existing cannabis research and are able to incorporate it into their communications with patients instead of leaving patients to figure out medical cannabis on their own.” “∆ 9 -Tetrahydrocannabinol (∆9 -THC), the active phytocannabinoid in cannabis, is virtually an adjunct to the endogenous endocannabinoid signaling system.
“∆ 9 -Tetrahydrocannabinol (∆9 -THC), the active phytocannabinoid in cannabis, is virtually an adjunct to the endogenous endocannabinoid signaling system. “Diabetes mellitus (DM), a metabolic disorder is one of the most prevalent chronic diseases worldwide across developed as well as developing nations. Hyperglycemia is the core feature of the type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM), following insulin deficiency and impaired insulin secretion or sensitivity leads insulin resistance (IR), respectively. Genetic and environmental factors attributed to the pathogenesis of DM and various therapeutic strategies are available for the prevention and treatment of T2DM.
“Diabetes mellitus (DM), a metabolic disorder is one of the most prevalent chronic diseases worldwide across developed as well as developing nations. Hyperglycemia is the core feature of the type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM), following insulin deficiency and impaired insulin secretion or sensitivity leads insulin resistance (IR), respectively. Genetic and environmental factors attributed to the pathogenesis of DM and various therapeutic strategies are available for the prevention and treatment of T2DM.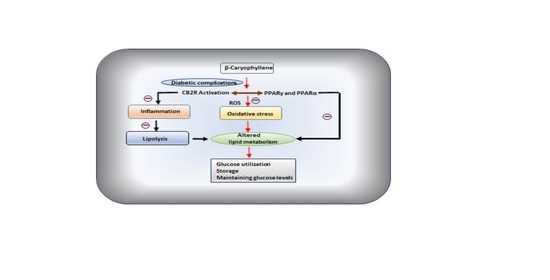
 “While activation of cannabinoid (CB2) receptors has been shown to be neuroprotective, no studies have examined whether this neuroprotection is directed at cerebral arterioles and no studies have examined whether activation of CB2 receptors can rescue cerebrovascular dysfunction during a chronic disease state such as type 1 diabetes (T1D).
“While activation of cannabinoid (CB2) receptors has been shown to be neuroprotective, no studies have examined whether this neuroprotection is directed at cerebral arterioles and no studies have examined whether activation of CB2 receptors can rescue cerebrovascular dysfunction during a chronic disease state such as type 1 diabetes (T1D). “Studies that have analyzed the association between cannabis use and acute ischemic stroke (AIS) have provided conflicting results.
“Studies that have analyzed the association between cannabis use and acute ischemic stroke (AIS) have provided conflicting results.
 “Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.
“Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.