 “Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
“Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
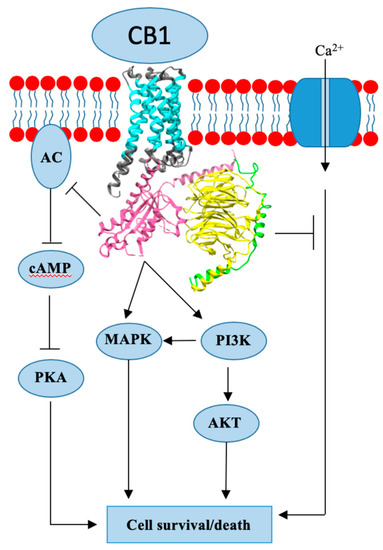
Endogenous cannabinoids together with cannabinoid receptor 1 and 2 (CB1, CB2) constitute the basis of the endocannabinoid system.
Interactions of cannabinoids with hypothalamic-pituitary-gonadal axis hormones are well documented, and two studies found a positive correlation between peak plasma endogenous cannabinoid anandamide with peak plasma 17β-estradiol, luteinizing hormone and follicle-stimulating hormone levels at ovulation in healthy premenopausal women. Do cannabinoids have an effect on HR+ BC? In this paper we review known and possible interactions between cannabinoids and specific HR+ BC treatments.
In preclinical studies, CB1 and CB2 agonists (i.e., anandamide, THC) have been shown to inhibit the proliferation of ER positive BC cell lines.
There is less evidence for antitumor cannabinoid action in HR+ BC in animal models and there are no clinical trials exploring the effects of cannabinoids on HR+ BC treatment outcomes. Two studies have shown that tamoxifen and several other selective estrogen receptor modulators (SERM) can act as inverse agonists on CB1 and CB2, an interaction with possible clinical consequences. In addition, cannabinoid action could interact with other commonly used endocrine and targeted therapies used in the treatment of HR+ BC.”
https://www.ncbi.nlm.nih.gov/pubmed/32106399
https://www.mdpi.com/2072-6694/12/3/525

 “Metastatic breast cancer is prevalent worldwide, and one of the most common sites of metastasis are long bones. Of patients with disease, the major symptom is pain, yet current medications fail to adequately result in analgesic efficacy and present major undesirable adverse effects.
“Metastatic breast cancer is prevalent worldwide, and one of the most common sites of metastasis are long bones. Of patients with disease, the major symptom is pain, yet current medications fail to adequately result in analgesic efficacy and present major undesirable adverse effects. “In recent years, the endocannabinoid system has received great interest as a potential therapeutic target in numerous pathological conditions.
“In recent years, the endocannabinoid system has received great interest as a potential therapeutic target in numerous pathological conditions. “Cannabidiol (CBD) has emerged as a potential agent for breast cancer management.
“Cannabidiol (CBD) has emerged as a potential agent for breast cancer management.
 “The anticancer effects of the omega-3 long chain polyunsaturated fatty acids (LCPUFA), EPA and DHA may be due, at least in part, to conversion to their respective endocannabinoid derivatives, eicosapentaenoyl-ethanolamine (EPEA) and docosahexaenoyl-ethanolamine (DHEA).
“The anticancer effects of the omega-3 long chain polyunsaturated fatty acids (LCPUFA), EPA and DHA may be due, at least in part, to conversion to their respective endocannabinoid derivatives, eicosapentaenoyl-ethanolamine (EPEA) and docosahexaenoyl-ethanolamine (DHEA). “Cannabinoids exhibit anti-inflammatory and antitumorigenic properties.
“Cannabinoids exhibit anti-inflammatory and antitumorigenic properties. “Indisputably, cancer is a global crisis that requires immediate intervention. Despite the use of conventional treatments over the past decades, it is acceptable to admit that these are expensive, invasive, associated with many side effects and, therefore, a reduced quality of life.
“Indisputably, cancer is a global crisis that requires immediate intervention. Despite the use of conventional treatments over the past decades, it is acceptable to admit that these are expensive, invasive, associated with many side effects and, therefore, a reduced quality of life.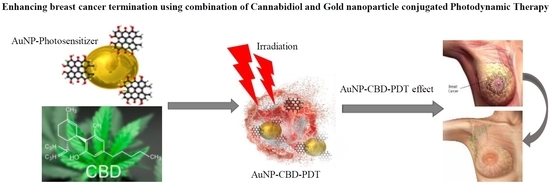
 “Phytocannabinoids are unique terpenophenolic compounds predominantly produced in the glandular trichomes of the cannabis plant (Cannabis sativa L.). The delta-9- tetrahydrocannabinol (THC) is the main active constituent responsible for the plant’s psychoactive effect and, together with the non- psychoactive cannabidiol (CBD), the most investigated naturally occurring cannabinoid.
“Phytocannabinoids are unique terpenophenolic compounds predominantly produced in the glandular trichomes of the cannabis plant (Cannabis sativa L.). The delta-9- tetrahydrocannabinol (THC) is the main active constituent responsible for the plant’s psychoactive effect and, together with the non- psychoactive cannabidiol (CBD), the most investigated naturally occurring cannabinoid. “Olivia Newton-John says medicinal marijuana is a key part of her treatment for stage four cancer. In an exclusive interview with 60 Minutes reporter Liz Hayes, Newton-John says that not only has cannabis assisted with her pain management, sleep and anxiety – but it’s having affects on her physical health too. “I’m incredibly pro cannabis,” she told Liz Hayes. “If I don’t take the cannabis, I can feel the pain so I know it’s working.”
“Olivia Newton-John says medicinal marijuana is a key part of her treatment for stage four cancer. In an exclusive interview with 60 Minutes reporter Liz Hayes, Newton-John says that not only has cannabis assisted with her pain management, sleep and anxiety – but it’s having affects on her physical health too. “I’m incredibly pro cannabis,” she told Liz Hayes. “If I don’t take the cannabis, I can feel the pain so I know it’s working.”
